LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Can you take weight loss injections after gastric sleeve surgery? Yes, weight loss injections such as semaglutide (Wegovy) and tirzepatide (Zepbound) can be prescribed after gastric sleeve surgery for appropriate candidates. While gastric sleeve surgery produces significant weight loss by removing approximately 80% of the stomach, some patients experience weight regain or fail to reach their target goals. FDA-approved GLP-1 and dual GIP/GLP-1 receptor agonists offer an additional therapeutic option when combined with bariatric surgery. However, this decision requires careful medical evaluation, proper timing, and close coordination with your bariatric surgery team to ensure safety and optimize outcomes.
Quick Answer: Weight loss injections can be prescribed after gastric sleeve surgery in appropriate candidates when evaluated and monitored by a bariatric surgery team.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Gastric sleeve surgery, or sleeve gastrectomy, is a highly effective bariatric procedure that removes approximately 80% of the stomach, creating a smaller, sleeve-shaped organ. While this surgery produces significant weight loss for most patients, some individuals experience weight regain or fail to reach their target weight goals in the years following surgery. This has led many patients and clinicians to consider adjunctive therapies, including weight loss injections.
Weight loss medications approved by the FDA specifically for chronic weight management include semaglutide (Wegovy) and tirzepatide (Zepbound). It's important to note that semaglutide (Ozempic) and tirzepatide (Mounjaro) are FDA-approved only for type 2 diabetes management, though they may sometimes be prescribed off-label for weight loss. Pharmacologically, semaglutide is a GLP-1 receptor agonist, while tirzepatide is a dual GIP/GLP-1 receptor agonist. These medications work by mimicking naturally occurring hormones that regulate appetite and blood sugar.
The short answer is yes—weight loss injections can be prescribed after gastric sleeve surgery in appropriate candidates, and emerging evidence suggests they may offer benefits for certain patients. However, this decision requires careful medical evaluation and coordination with your bariatric surgery team. The combination of surgical and pharmacological interventions represents a newer approach to managing complex obesity, and understanding the interplay between these treatments is essential for patient safety and optimal outcomes. Each patient's situation is unique, and factors such as time since surgery, current weight status, comorbidities, and individual response to the sleeve procedure all influence whether weight loss injections are appropriate.
The timing of initiating weight loss injections after gastric sleeve surgery should be individualized based on clinical circumstances. Many bariatric specialists consider these medications when patients experience a weight loss plateau or early weight regain despite adherence to dietary and lifestyle recommendations. This typically occurs after the period of rapid post-surgical weight loss has stabilized.
During the initial post-operative period, patients experience rapid weight loss as they adjust to their reduced stomach capacity and follow a structured dietary progression. Introducing weight loss medications too early may complicate this adjustment phase and make it difficult to distinguish the effects of surgery from those of medication. Additionally, the early post-operative period carries its own risks of nausea, vomiting, and gastrointestinal symptoms—side effects that overlap significantly with those of GLP-1 and GIP/GLP-1 medications.
Safety considerations include assessing for potential complications from the original surgery, ensuring adequate nutritional status, and evaluating kidney and liver function. Patients must be metabolically stable, meeting their protein and micronutrient goals, and free from active complications such as strictures or ulcers before starting these medications.
Important contraindications include personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 (MEN2), history of pancreatitis, severe gastrointestinal disease including gastroparesis, and pregnancy or planned pregnancy (these medications should be discontinued at least 2 months before a planned pregnancy). Your bariatric team will conduct appropriate laboratory testing and clinical assessments to determine if these medications are suitable for your individual situation.
Patients should seek immediate medical attention for warning signs including persistent vomiting, inability to keep fluids down, severe or radiating abdominal pain, right upper quadrant pain with fever, or signs of hypoglycemia (if taking diabetes medications).
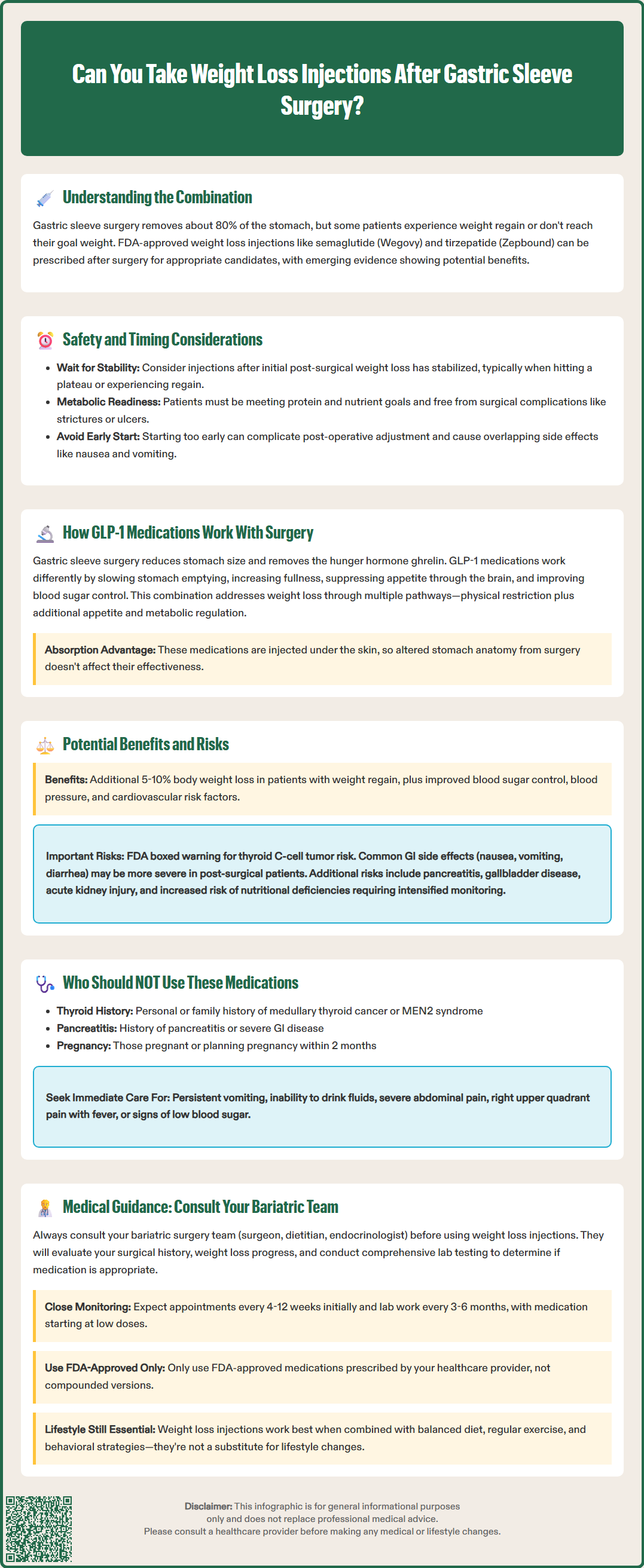
Understanding the mechanisms of both gastric sleeve surgery and weight loss medications reveals why they may work in complementary ways. Gastric sleeve surgery achieves weight loss through multiple mechanisms: it mechanically restricts food intake by reducing stomach volume, removes the fundus (which produces the hunger hormone ghrelin), and alters gut hormone secretion. These changes lead to reduced appetite, earlier satiety, and metabolic improvements including enhanced insulin sensitivity.
GLP-1 receptor agonists like semaglutide work through distinct pathways. These medications mimic glucagon-like peptide-1, an incretin hormone naturally released by the intestines in response to food intake. GLP-1 slows gastric emptying, increases satiety, reduces appetite through central nervous system effects, and enhances glucose-dependent insulin secretion while suppressing glucagon release. Tirzepatide adds activation of the glucose-dependent insulinotropic polypeptide (GIP) receptor, providing additional metabolic benefits. Interestingly, gastric sleeve surgery itself increases endogenous GLP-1 levels, which contributes to its metabolic benefits.
The combination of surgical and pharmacological approaches may address different aspects of weight regulation. While the sleeve provides a physical restriction and alters gut hormone profiles, these medications add an additional layer of appetite suppression and metabolic regulation. This complementary approach may be particularly beneficial for patients whose endogenous GLP-1 response to surgery is insufficient or diminishes over time.
These medications are administered subcutaneously, bypassing the gastrointestinal tract, so their absorption is not affected by the altered anatomy from gastric sleeve surgery. This route of administration helps maintain consistent drug delivery and effectiveness, though individual responses vary. Current evidence generally supports that these medications can be effective after bariatric procedures, though more research is needed on their long-term outcomes in post-bariatric populations.
The potential benefits of adding weight loss injections after gastric sleeve surgery can be significant for appropriately selected patients. Clinical studies have demonstrated that these medications can produce additional weight loss in post-bariatric patients who have experienced weight regain or inadequate initial weight loss. Patients may achieve additional weight loss, typically around 5-10% of their body weight, though results vary considerably between individuals.
Beyond weight loss, these medications offer metabolic benefits that complement those achieved through surgery. These include improved glycemic control in patients with type 2 diabetes, reductions in blood pressure, and favorable effects on cardiovascular risk factors. For patients whose obesity-related comorbidities have not fully resolved after surgery or have recurred with weight regain, these medications may provide additional therapeutic value. Some evidence also suggests potential benefits for metabolic dysfunction-associated steatotic liver disease (MASLD, formerly known as NAFLD), a common comorbidity in obesity.
However, combining these treatments also carries specific risks that require careful consideration. The FDA-approved labels for these medications include a boxed warning about the risk of thyroid C-cell tumors, and they are contraindicated in patients with a personal or family history of medullary thyroid carcinoma or MEN2. Common side effects include nausea, vomiting, diarrhea, and constipation—which can be particularly problematic in post-surgical patients who already have altered gastrointestinal anatomy and function. The combination of reduced stomach capacity and medication-induced delayed gastric emptying may increase the risk of severe nausea or vomiting, potentially leading to dehydration or nutritional deficiencies.
Additional risks include pancreatitis, gallbladder disease, acute kidney injury from dehydration, and potential worsening of diabetic retinopathy in patients with diabetes who experience rapid improvement in blood glucose. Patients taking insulin or sulfonylureas may need dose adjustments to prevent hypoglycemia. There is also concern about the potential for excessive or rapid weight loss when combining treatments, which may increase the risk of nutritional deficiencies, particularly in protein, vitamins, and minerals. Post-bariatric patients already require lifelong supplementation and monitoring; adding weight loss medications necessitates even more vigilant nutritional surveillance. Additionally, the cost of these medications can be substantial, and insurance coverage varies. Patients should also be aware of the potential for weight regain if medications are discontinued, emphasizing the importance of sustained lifestyle modifications regardless of treatment modality.
The decision to use weight loss injections after gastric sleeve surgery should never be made independently. Your bariatric surgery team—including your surgeon, dietitian, and potentially an endocrinologist or obesity medicine specialist—must be involved in this decision-making process. These professionals understand your surgical history, current health status, and individual risk factors, enabling them to provide personalized recommendations.
Before considering weight loss injections, your bariatric team will conduct a comprehensive evaluation. This includes reviewing your weight loss trajectory since surgery, assessing adherence to dietary and lifestyle recommendations, and evaluating for any anatomical or functional complications from the surgery. Laboratory testing will assess nutritional status, including protein levels, vitamin and mineral stores, kidney function, and metabolic parameters. Typical monitoring includes complete blood count, comprehensive metabolic panel, iron studies/ferritin, vitamin B12, folate, vitamin D, thiamine, calcium/PTH, lipid panel, and hemoglobin A1c. Your team will also review your current medications, as drug interactions and contraindications must be considered.
If weight loss injections are deemed appropriate, your team will develop a monitoring plan that includes regular follow-up appointments (typically every 4-12 weeks initially), ongoing nutritional counseling, and laboratory surveillance every 3-6 months. The medication will typically be started at a low dose and gradually titrated to minimize side effects while optimizing efficacy. Your dietitian will work with you to ensure adequate protein and nutrient intake despite potentially reduced appetite, and may adjust your supplementation regimen accordingly.
For safety reasons, you should only use FDA-approved medications prescribed by your healthcare provider. The FDA has issued warnings about compounded versions of these medications, which may not meet quality standards. Your healthcare team will provide training on proper injection technique, storage requirements, and safe disposal of used needles.
It is essential to maintain realistic expectations and understand that weight loss medications are not a substitute for the lifestyle modifications that are fundamental to long-term success after bariatric surgery. These medications work best as part of a comprehensive approach that includes a balanced diet, regular physical activity, behavioral strategies, and ongoing medical support. Your bariatric team will help you understand the expected outcomes, potential side effects, duration of treatment, and criteria for discontinuation. Open communication with your healthcare providers about your experiences, concerns, and goals is crucial for achieving the best possible outcomes while minimizing risks.
Weight loss injections are typically considered after the initial rapid post-operative weight loss period has stabilized, usually when patients experience a weight plateau or early weight regain despite adherence to dietary and lifestyle recommendations. Your bariatric team will determine the appropriate timing based on your metabolic stability, nutritional status, and absence of surgical complications.
Weight loss injections can be safe after gastric sleeve surgery when prescribed and monitored by your bariatric team, but they carry specific risks including nausea, vomiting, and potential nutritional deficiencies. Contraindications include personal or family history of medullary thyroid carcinoma or MEN2, history of pancreatitis, and pregnancy.
Insurance coverage for weight loss medications after bariatric surgery varies considerably between plans and depends on factors such as medical necessity, specific indications, and policy terms. Patients should consult with their insurance provider and bariatric team to understand coverage options and potential out-of-pocket costs.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.