LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Do GLP-1 medications give you energy? This question arises frequently as more patients begin glucagon-like peptide-1 (GLP-1) receptor agonists like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound) for type 2 diabetes and weight management. While these medications don't directly stimulate energy production, many patients report feeling more energetic through improved blood sugar control and weight loss. Conversely, fatigue is a recognized side effect, particularly during initial treatment. Understanding how GLP-1 therapy affects energy levels—both positively and negatively—helps patients and clinicians optimize treatment outcomes and manage expectations during therapy.
Quick Answer: GLP-1 medications do not directly increase energy but may improve perceived energy through better blood sugar control and weight loss, though fatigue is also a common side effect.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed for type 2 diabetes management and now widely prescribed for chronic weight management. These agents include semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and exenatide (Byetta, Bydureon). Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist with similar clinical effects. These medications mimic the action of naturally occurring GLP-1, an incretin hormone released by the intestine in response to food intake.
The primary mechanism of action involves binding to GLP-1 receptors in multiple tissues throughout the body. In the pancreas, these medications enhance glucose-dependent insulin secretion and suppress inappropriate glucagon release, thereby improving glycemic control. In the gastrointestinal tract, they slow gastric emptying, which prolongs satiety and reduces appetite. Central nervous system effects include actions on hypothalamic appetite centers, contributing to reduced caloric intake and subsequent weight loss.
These medications do not directly target cellular energy production or mitochondrial function. Their effects on energy levels are indirect, mediated through improvements in metabolic parameters, weight reduction, and glycemic stability. The FDA-approved indications focus on glycemic control in type 2 diabetes and chronic weight management in adults with obesity or overweight with at least one weight-related comorbidity, with some products (Wegovy, Saxenda) also approved for certain adolescents. When combined with insulin or sulfonylureas, these medications increase the risk of hypoglycemia, which may require dose adjustments of those agents.
Many patients report subjective improvements in energy levels after initiating GLP-1 therapy, though this effect is not universal and reflects multiple contributing factors rather than direct pharmacological stimulation. The most significant contributor is improved glycemic control in patients with type 2 diabetes. Chronic hyperglycemia often causes fatigue, polyuria, and general malaise; as GLP-1 medications stabilize blood glucose levels and reduce glycemic variability, patients frequently experience resolution of these symptoms and perceive increased vitality.
Weight loss achieved through GLP-1 therapy contributes substantially to improved energy perception. Excess adiposity, particularly in the context of obesity, is associated with increased mechanical load during physical activity, sleep-disordered breathing, and systemic inflammation—all of which contribute to fatigue. As patients lose weight, many report enhanced mobility, improved sleep quality, and greater ease performing daily activities. Clinical trials such as the STEP program (semaglutide) and SURMOUNT trials (tirzepatide) have demonstrated improvements in physical functioning and quality of life scores, which patients often interpret as increased energy.
Additionally, improvements in weight-related comorbidities may enhance overall well-being. Weight loss can improve obstructive sleep apnea, joint pain, and cardiovascular function, which may indirectly boost energy levels. Some patients also report psychological benefits, including improved mood and motivation, which may relate to achieving weight loss goals and improved self-efficacy. However, it is important to note that there is no official pharmacological mechanism by which GLP-1 medications directly increase cellular energy production or act as stimulants. The perceived energy boost represents a secondary benefit of metabolic optimization rather than a primary drug effect.
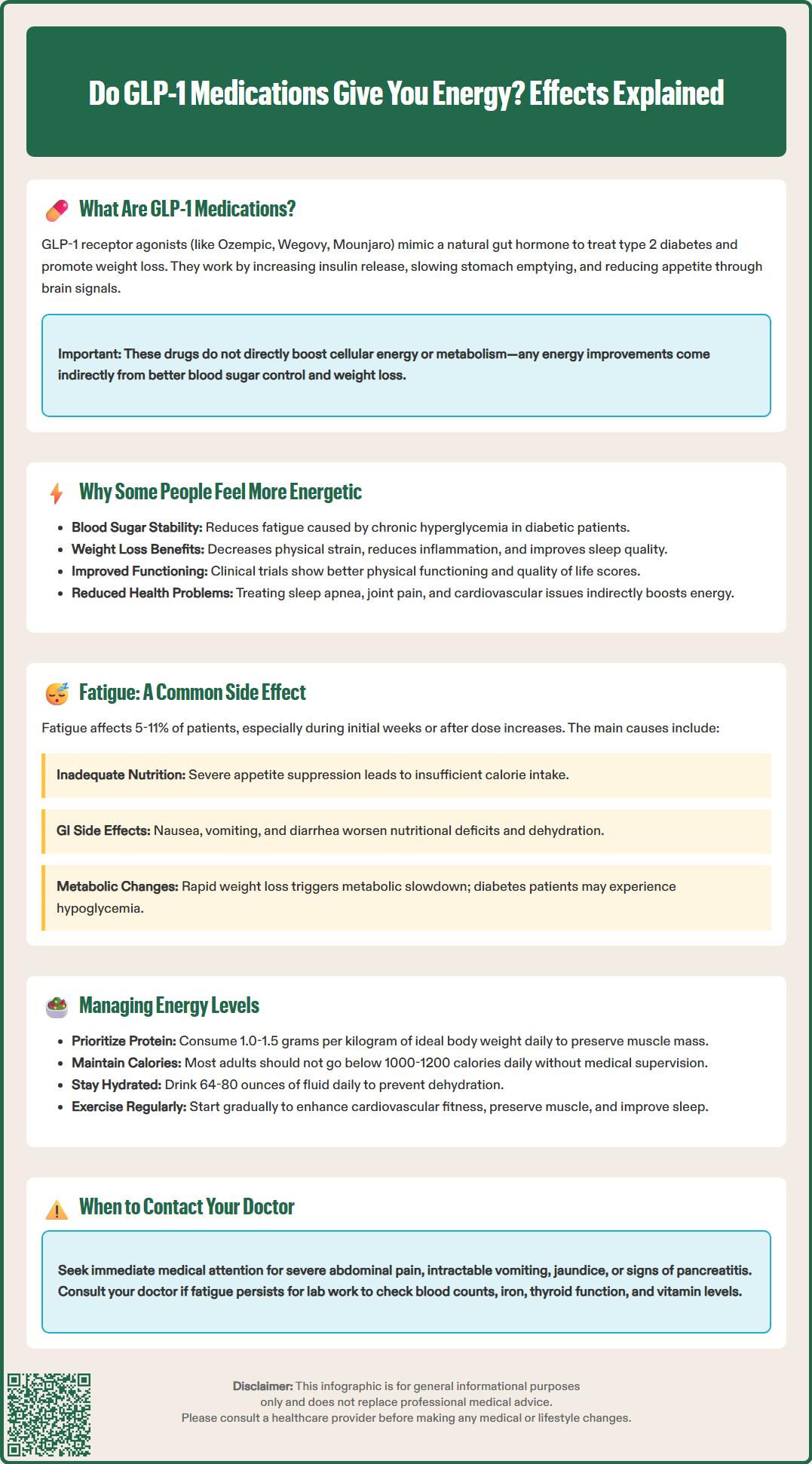
Paradoxically, fatigue is among the commonly reported adverse effects of GLP-1 therapy, particularly during the initial weeks of treatment or following dose escalation. Clinical trial data and post-marketing surveillance indicate that a subset of patients experience decreased energy, tiredness, and general malaise while taking these medications. The FDA prescribing information for semaglutide and tirzepatide lists fatigue as an adverse reaction occurring in clinical studies, with incidence rates typically ranging from 5-11% depending on the specific product and dosage.
Several mechanisms may contribute to GLP-1-associated fatigue. The most significant is the substantial caloric restriction that occurs as appetite suppression takes effect. Patients often experience significant reductions in food intake, which can lead to insufficient energy substrate availability, particularly if nutritional quality is poor. Gastrointestinal side effects, including nausea, vomiting, and diarrhea, are extremely common with GLP-1 therapy and may exacerbate nutritional deficits while directly contributing to feelings of unwellness and fatigue.
Dehydration represents another important contributor, as reduced oral intake due to nausea or early satiety combined with gastrointestinal losses can lead to volume depletion. Rapid weight loss itself may trigger adaptive metabolic responses, including reduced resting metabolic rate, which some patients perceive as low energy. In patients with diabetes, overly aggressive glycemic control or inadequate adjustment of concurrent diabetes medications (particularly insulin or sulfonylureas) may result in hypoglycemia or relative hypoglycemia, even if glucose values remain within normal range. Slow dose titration and temporary dose reductions can help lessen fatigue and GI symptoms. Clinicians should systematically evaluate these potential causes when patients report persistent fatigue during GLP-1 therapy, as many are modifiable through dietary counseling, hydration strategies, or medication adjustment.
Optimizing energy levels during GLP-1 therapy requires a systematic approach addressing nutrition, hydration, physical activity, and medication management. Patients should prioritize protein intake to preserve lean body mass during weight loss, aiming for 1.0-1.5 grams per kilogram of ideal body weight daily (lower for those with chronic kidney disease), distributed across meals. Despite reduced appetite, maintaining adequate caloric intake is important to prevent excessive fatigue. Calorie needs should be individualized based on sex, size, and activity level, with most adults avoiding intake below 1000-1200 calories daily without medical supervision. Small, frequent meals may be better tolerated than larger portions given the delayed gastric emptying induced by GLP-1 medications.
Hydration requires particular attention, as patients may experience reduced oral intake due to nausea or early satiety. A target of 64-80 ounces of fluid daily is appropriate for most patients (with adjustments for heart failure or kidney disease), with modifications based on activity level, climate, and gastrointestinal losses. Electrolyte solutions may be beneficial when vomiting or diarrhea are present. Regular physical activity, even at modest intensity, can paradoxically improve energy levels by enhancing cardiovascular fitness, preserving muscle mass, and improving sleep quality. Patients should be counseled to start gradually and increase activity as tolerated.
Clinicians should conduct targeted investigations when fatigue persists beyond the initial adjustment period. Laboratory evaluation may include complete blood count, iron studies (ferritin, iron, TIBC), comprehensive metabolic panel, thyroid function tests, and vitamin B12 and vitamin D levels. In patients with diabetes, review of glucose monitoring data can identify problematic glycemic patterns. Medication review is essential—dose reduction or temporary discontinuation may be necessary if side effects are severe, and concurrent medications (particularly insulin or sulfonylureas) may require adjustment.
Patients should stop the medication and seek immediate medical attention for severe, persistent abdominal pain, intractable vomiting, jaundice, or signs of pancreatitis or gallbladder disease. Patients should also be informed about the boxed warning regarding medullary thyroid carcinoma risk, the importance of avoiding these medications during pregnancy and lactation, and the need for appropriate monitoring if rapid improvements in blood glucose occur in patients with diabetes and retinopathy.
No, GLP-1 medications do not directly stimulate cellular energy production or act as stimulants. Any perceived energy increase results indirectly from improved blood sugar control, weight loss, and resolution of obesity-related symptoms rather than pharmacological stimulation.
Fatigue affects 5-11% of patients and typically results from substantial caloric restriction due to appetite suppression, gastrointestinal side effects like nausea and vomiting, dehydration from reduced oral intake, or rapid metabolic changes during weight loss.
Prioritize adequate protein intake (1.0-1.5 g/kg daily), maintain hydration with 64-80 ounces of fluid daily, avoid dropping below 1000-1200 calories without medical supervision, and engage in regular physical activity. If fatigue persists, consult your clinician for laboratory evaluation and possible medication adjustment.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.