LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide (Mounjaro, Zepbound) is a once-weekly injectable medication FDA-approved for type 2 diabetes and chronic weight management. As a dual GIP/GLP-1 receptor agonist, it works by enhancing insulin secretion, suppressing glucagon, and slowing gastric emptying. Many patients wonder whether tirzepatide needs to be taken on an empty stomach. Unlike oral medications that require specific meal timing, tirzepatide is administered as a subcutaneous injection and can be given at any time of day, regardless of meals. Understanding proper administration timing helps patients establish consistent routines and optimize treatment adherence while minimizing potential side effects.
Quick Answer: Tirzepatide does not need to be taken on an empty stomach and can be injected at any time of day, regardless of meals.
Tirzepatide (Mounjaro, Zepbound) is a once-weekly subcutaneous injection approved by the FDA for type 2 diabetes management and chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. As a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist, tirzepatide enhances insulin secretion, suppresses glucagon release, and slows gastric emptying to improve glycemic control and promote weight loss.
The medication is administered subcutaneously into the abdomen, thigh, or upper arm (upper arm injections typically require administration by another person) using a single-dose prefilled pen. Patients should inject tirzepatide once weekly on the same day each week, at any time of day that is convenient and sustainable for their routine. The injection site should be rotated with each dose to minimize local reactions such as erythema, induration, or discomfort at the injection site.
Initial dosing typically begins at 2.5 mg once weekly for four weeks as a treatment initiation dose to improve gastrointestinal tolerability. The dose is then increased to 5 mg once weekly, with further escalation in 2.5 mg increments every four weeks as needed, based on glycemic response and tolerability, up to a maximum of 15 mg once weekly. Dose escalation should be individualized, and patients should be counseled that the starting dose is not therapeutic for glycemic control but rather intended to reduce gastrointestinal adverse effects during treatment initiation.
Important: Tirzepatide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Tirzepatide is not indicated for type 1 diabetes and should not be used in combination with other GLP-1 receptor agonists or DPP-4 inhibitors.
Tirzepatide does not need to be taken on an empty stomach. Unlike some oral medications that require specific timing relative to meals for optimal absorption, tirzepatide is administered as a subcutaneous injection, which bypasses the gastrointestinal tract for absorption. The medication can be injected at any time of day, regardless of meal timing, without affecting its pharmacokinetics or therapeutic efficacy.
Clinical pharmacology studies demonstrate that tirzepatide absorption is not influenced by food intake. The subcutaneous route delivers the medication directly into the adipose tissue, from which it is absorbed into the systemic circulation independent of gastric contents or digestive processes. Peak plasma concentrations are typically reached 8 to 72 hours post-injection, with a half-life of approximately five days, supporting once-weekly dosing.
Patients may choose to administer tirzepatide before, during, or after meals based on personal preference and what best fits their weekly routine. Some patients prefer injecting in the morning as part of their routine, while others find evening administration more convenient. The key consideration is consistency—selecting the same day each week and a time that the patient can reliably remember. If a dose is missed, it should be administered as soon as possible within four days (96 hours) after the missed dose. If more than four days have passed, the missed dose should be skipped, and the next dose should be administered on the regularly scheduled day.
If a patient needs to change their regular injection day, they may do so as long as the time between doses is at least three days (72 hours). The new day then becomes the regular weekly schedule going forward.
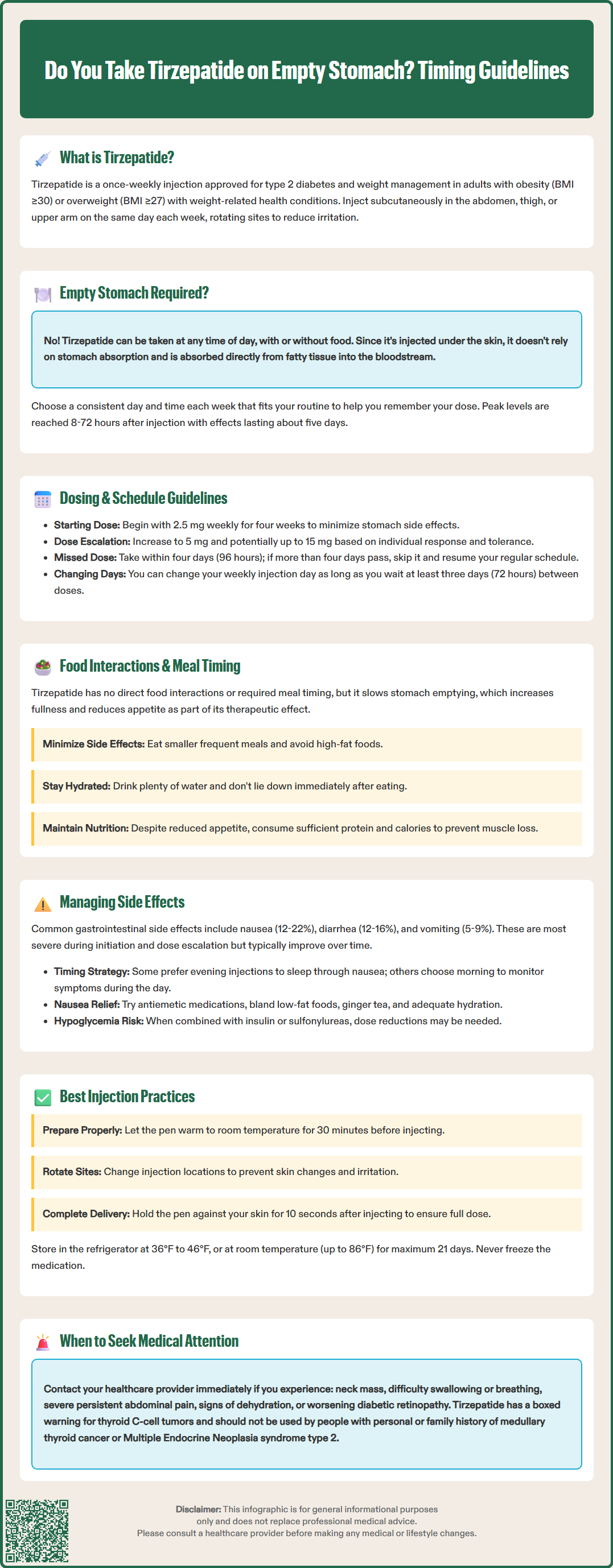
Tirzepatide has no direct food interactions that require dietary restrictions or specific meal timing for injection administration. However, the medication's mechanism of action significantly affects how the body processes food, which has important implications for patient counseling and dietary management.
As a GIP/GLP-1 receptor agonist, tirzepatide delays gastric emptying, which slows the rate at which food moves from the stomach into the small intestine. This physiological effect contributes to increased satiety, reduced appetite, and improved postprandial glucose excursion. Patients commonly report feeling fuller for longer periods after meals and experiencing reduced hunger between meals. These effects are therapeutic and contribute to both glycemic control and weight loss outcomes observed in clinical trials.
This delayed gastric emptying can affect the absorption of oral medications, particularly those with narrow therapeutic indices or requiring rapid gastrointestinal absorption. Notably, tirzepatide may reduce the effectiveness of oral contraceptives. Patients using oral contraceptives should use a non-oral or backup contraceptive method for 4 weeks after tirzepatide initiation and after each dose increase.
Tirzepatide is not recommended for patients with severe gastrointestinal disease, including severe gastroparesis, due to its effects on gastric emptying.
Patients should be counseled about potential gastrointestinal symptoms related to delayed gastric emptying, particularly during dose escalation. Eating large, high-fat meals may exacerbate feelings of fullness, nausea, or abdominal discomfort. Practical dietary recommendations include consuming smaller, more frequent meals; avoiding lying down immediately after eating; limiting high-fat and fried foods; staying well-hydrated throughout the day; and moderating alcohol consumption to reduce pancreatitis risk.
There are no absolute dietary restrictions with tirzepatide, but patients should maintain adequate nutritional intake despite reduced appetite. Consultation with a registered dietitian can help patients develop meal plans that support therapeutic goals while ensuring sufficient protein, micronutrients, and overall caloric intake to prevent excessive muscle loss during weight reduction. Patients with diabetes should continue monitoring blood glucose levels and adjust other diabetes medications as directed by their healthcare provider to prevent hypoglycemia.
The most common adverse effects of tirzepatide are gastrointestinal in nature, occurring in a dose-dependent manner and typically most pronounced during treatment initiation and dose escalation. In clinical trials, nausea (12-22%), diarrhea (12-16%), vomiting (5-9%), constipation (6-7%), abdominal pain (6-9%), and dyspepsia (7-10%) were frequently reported. These effects generally diminish over time as patients develop tolerance to the medication.
While injection timing relative to meals does not affect tirzepatide absorption, some patients report that timing their injection may influence the severity or perception of gastrointestinal symptoms. There is no official guidance on optimal timing to minimize side effects, as individual responses vary considerably. Some patients find that injecting in the evening allows them to sleep through peak nausea periods, while others prefer morning administration to monitor for adverse effects during waking hours.
Patients experiencing significant nausea should consult their healthcare provider, who may prescribe antiemetic medications such as ondansetron. If prescribed, metoclopramide should be used with caution and for short durations due to the risk of tardive dyskinesia and other neurological side effects.
Non-pharmacological strategies include eating bland, low-fat foods; avoiding strong odors; consuming ginger tea; and ensuring adequate hydration. If vomiting is severe or persistent, patients should be evaluated for dehydration and electrolyte disturbances.
Other notable adverse effects include injection site reactions (typically mild and self-limiting), fatigue, and potential hypoglycemia when used with insulin or sulfonylureas. Doses of insulin or sulfonylureas may need to be reduced when initiating or escalating tirzepatide to reduce hypoglycemia risk.
Patients should be monitored for serious adverse effects including:
Thyroid tumors (boxed warning): Report symptoms such as neck mass, dysphagia, dyspnea, or persistent hoarseness
Pancreatitis: Discontinue if suspected; severe persistent abdominal pain, sometimes radiating to the back, with or without vomiting
Gallbladder disease
Acute kidney injury (usually secondary to dehydration from gastrointestinal symptoms)
Hypersensitivity reactions
Worsening of diabetic retinopathy in patients with pre-existing retinopathy
For weight management patients (Zepbound): Monitor for depression or suicidal thoughts
Establishing a consistent, sustainable injection schedule is essential for treatment adherence and optimal therapeutic outcomes with tirzepatide. Patients should select a specific day of the week that aligns with their routine and set reminders to ensure doses are not missed. Many patients find it helpful to coordinate their injection day with existing weekly activities or appointments as a memory aid.
The injection can be administered at any time on the scheduled day, and patients do not need to inject at the same time each week—only the same day matters for maintaining steady-state drug levels. If a patient needs to change their regular injection day, they may do so as long as the time between doses is at least three days (72 hours). The new day then becomes the regular weekly schedule going forward.
Proper injection technique is critical for medication efficacy and minimizing local reactions. Patients should:
Inspect the medication for particulate matter or discoloration before use (solution should be clear to slightly yellow)
Allow the pen to reach room temperature (30 minutes out of refrigerator) to reduce injection discomfort
Clean the injection site with an alcohol swab and allow to dry
Rotate injection sites systematically to prevent lipohypertrophy
Inject at a 90-degree angle, holding the pen firmly against the skin
Keep the pen pressed against the skin until the injection is complete (about 10 seconds) as indicated by the plunger stopping or the indicator showing completion
Never share pens or needles with others, even if the needle has been changed
Dispose of used pens in an FDA-cleared sharps container
Injections in the upper arm typically require administration by another person.
Tirzepatide should be stored in the refrigerator at 36°F to 46°F (2°C to 8°C) and protected from light. Unopened pens may be stored at room temperature up to 86°F (30°C) for up to 21 days. The medication should never be frozen, and pens should be discarded if freezing occurs. Patients should inspect their injection pens regularly and discard any that appear damaged or have been stored improperly. Healthcare providers should provide comprehensive injection training at treatment initiation and periodically reassess technique to ensure proper administration.
Yes, you can eat before or after your tirzepatide injection. Since tirzepatide is administered subcutaneously, food intake does not affect its absorption or effectiveness, allowing you to inject at any time regardless of meals.
Tirzepatide can be injected at any time of day on your scheduled weekly injection day. The key is consistency—choose the same day each week and a time that fits your routine and helps you remember to take your dose.
Yes, tirzepatide delays gastric emptying, which slows how food moves from the stomach to the small intestine. This contributes to increased satiety and reduced appetite, helping with both blood sugar control and weight management.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.