LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
When should you go up on tirzepatide? This decision depends on your therapeutic response, tolerability, and individual health goals. Tirzepatide, a dual GIP and GLP-1 receptor agonist approved for type 2 diabetes and chronic weight management, follows a structured titration schedule with dose increases typically occurring every four weeks. Understanding when to escalate from your current dose requires collaboration with your healthcare provider, assessment of glycemic control or weight management progress, and careful evaluation of side effects. This guide explains the clinical indicators, safety considerations, and timing factors that determine appropriate dose advancement.
Quick Answer: Tirzepatide dose increases typically occur every four weeks when glycemic targets or weight management goals are not met, gastrointestinal side effects have resolved, and the patient demonstrates good medication adherence.
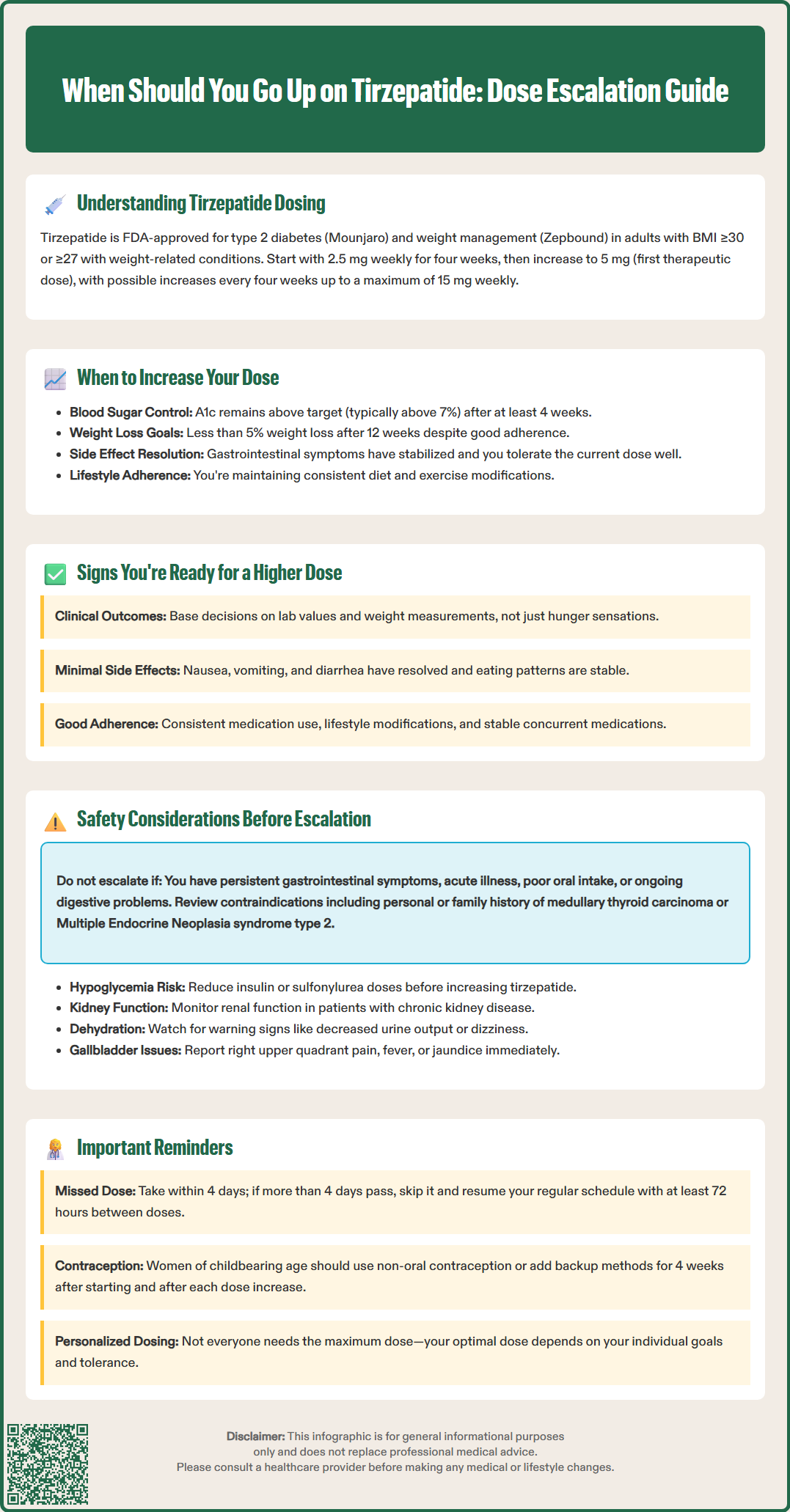
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound) in adults with BMI ≥30 kg/m², or ≥27 kg/m² with at least one weight-related comorbidity.
The standard titration schedule begins with a starting dose of 2.5 mg administered subcutaneously once weekly. This initial dose serves primarily as a tolerability-building phase rather than a therapeutic dose. After four weeks at 2.5 mg, patients typically advance to 5 mg weekly, which represents the first recommended maintenance dose for glycemic control. Subsequent dose increases occur in 2.5 mg increments at four-week intervals, progressing through 7.5 mg, 10 mg, 12.5 mg, and reaching a maximum of 15 mg weekly. The FDA-recommended maintenance doses are 5 mg, 10 mg, or 15 mg once weekly, with 7.5 mg and 12.5 mg primarily serving as intermediate steps to improve tolerability.
This gradual titration protocol is designed to allow physiological adaptation to the medication's effects on gastric emptying and satiety signaling. The four-week interval between dose adjustments provides sufficient time to assess therapeutic response, evaluate tolerability, and monitor for adverse effects. This stepwise approach used in clinical trials aims to improve gastrointestinal tolerability.
If a dose is missed, it should be administered within 4 days of the scheduled dose. If more than 4 days have passed, skip the missed dose and administer the next dose on the regularly scheduled day. In either case, patients can then resume their regular once-weekly dosing schedule, ensuring at least 72 hours between doses.
Patients should understand that tirzepatide dosing is individualized based on glycemic targets, weight management goals, and tolerability. Not all patients require maximum dosing, and some achieve optimal results at intermediate doses. Concomitant use with other GLP-1 receptor agonists or incretin-based therapies is not recommended, as this combination has not been studied.
Dose escalation decisions should be made collaboratively between patients and healthcare providers, typically occurring after completing at least four weeks at the current dose. The primary indication for increasing tirzepatide is inadequate therapeutic response, defined as failure to achieve individualized glycemic targets or weight management goals despite good medication adherence and lifestyle modifications.
For patients with type 2 diabetes, dose advancement is considered when hemoglobin A1c remains above target (typically 7% for most adults, though individualized based on patient factors) or when fasting and postprandial glucose levels exceed goals. The American Diabetes Association recommends reassessing glycemic control approximately three months after initiating or adjusting glucose-lowering therapy, though preliminary assessment of tolerability and response can occur earlier. When available, continuous glucose monitoring metrics such as time-in-range can provide valuable data to guide dose adjustment decisions. If A1c reduction is insufficient after adequate time at a given dose, escalation to the next tier is appropriate.
In the context of chronic weight management, dose increases may be warranted when weight loss is insufficient or plateaus before reaching clinically meaningful targets. Clinical guidelines suggest considering treatment modification if less than 5% weight loss occurs after approximately 12 weeks on a therapeutic dose. Clinical trials showed dose-dependent weight reduction, with higher doses producing greater average weight loss.
Timing considerations include ensuring the patient has tolerated the current dose well, with resolution or stabilization of any initial gastrointestinal symptoms. Dose escalation should not occur during acute illness, periods of poor oral intake, or when gastrointestinal symptoms from the current dose remain problematic. For patients using insulin or sulfonylureas, proactive dose reduction of these medications should be considered before tirzepatide escalation to mitigate hypoglycemia risk, with increased glucose monitoring during the transition.
Several clinical indicators suggest readiness for tirzepatide dose escalation. The most objective marker is laboratory evidence of suboptimal glycemic control, including hemoglobin A1c values above individualized targets or persistent hyperglycemia on self-monitoring blood glucose data. Patients should review glucose patterns with their healthcare provider, looking specifically at fasting glucose levels and two-hour postprandial readings to identify inadequate response.
For weight management, specific signs include insufficient weight loss despite continued medication adherence and lifestyle efforts, or failure to achieve clinically meaningful weight reduction within the expected timeframe. While changes in appetite and hunger may occur, treatment decisions should be based primarily on objective clinical outcomes rather than subjective hunger sensations.
Tolerance indicators are equally important in determining readiness for dose advancement. Patients should experience minimal or no gastrointestinal symptoms at their current dose, with resolution of initial nausea, vomiting, or diarrhea. Stable eating patterns, normal bowel function, and absence of persistent abdominal discomfort suggest adequate adaptation to the current dose. Additionally, patients should feel confident in their injection technique and weekly administration routine.
Patients ready for dose escalation typically demonstrate good medication adherence and have implemented recommended lifestyle modifications including dietary changes and increased physical activity. They should also have stable concurrent medications, with no recent changes to other glucose-lowering agents or medications affecting gastrointestinal function.
Women of childbearing potential should be aware that tirzepatide may reduce the effectiveness of oral contraceptives, particularly during dose initiation and escalation. Use of an alternative or additional non-oral contraceptive method is recommended for 4 weeks after initiating tirzepatide and for 4 weeks after each dose increase.
Before increasing tirzepatide dosage, several safety assessments are essential. Healthcare providers should review the patient's complete medical history, with particular attention to contraindications including personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. Patients should be counseled to report symptoms suggestive of thyroid tumors, including neck mass, dysphagia, hoarseness, or persistent dyspnea.
Patients with a history of pancreatitis require careful evaluation, as GLP-1 receptor agonists have been associated with pancreatitis risk, though causality remains uncertain. Tirzepatide is also associated with gallbladder disease (cholelithiasis, cholecystitis); patients should be advised to report symptoms such as right upper quadrant pain, fever, or jaundice for prompt evaluation.
Gastrointestinal tolerability must be thoroughly assessed before dose advancement. Persistent nausea, vomiting, or diarrhea at the current dose contraindicates escalation until symptoms resolve. Tirzepatide is not recommended for patients with severe gastrointestinal disease, including severe gastroparesis. Severe gastrointestinal adverse effects can lead to dehydration and acute kidney injury, particularly in patients with underlying renal impairment. Patients should be counseled on warning signs including inability to tolerate oral fluids, decreased urine output, dizziness, or severe abdominal pain, which require immediate medical evaluation rather than dose escalation.
Renal function monitoring is important in patients with pre-existing chronic kidney disease and when severe gastrointestinal adverse reactions occur that could lead to dehydration. Patients using insulin or insulin secretagogues (such as sulfonylureas) face increased hypoglycemia risk with tirzepatide dose increases. Proactive dose reduction of these concurrent agents is often necessary before tirzepatide escalation.
Women of childbearing potential should use effective contraception during tirzepatide treatment. Due to reduced oral contraceptive effectiveness, non-oral or additional contraceptive methods are recommended for 4 weeks after initiating tirzepatide and for 4 weeks after each dose increase. Tirzepatide should be discontinued if pregnancy is recognized. Patients should also be monitored for hypersensitivity reactions, including anaphylaxis and angioedema, and the medication discontinued if these occur.
You should wait at least four weeks at your current dose before considering an increase. This interval allows adequate time to assess therapeutic response, evaluate tolerability, and monitor for adverse effects.
Signs include hemoglobin A1c remaining above your individualized target, persistent hyperglycemia on glucose monitoring, or insufficient weight loss despite good medication adherence and lifestyle modifications. Your healthcare provider will assess these factors along with your tolerability of the current dose.
No, persistent nausea or other gastrointestinal symptoms at your current dose indicate you should not escalate until these symptoms resolve. Dose increases should only occur when you tolerate your current dose well with minimal or no side effects.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.