LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Many patients with Hashimoto's disease struggle with weight management and metabolic challenges, leading to questions about whether GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) or tirzepatide (Mounjaro, Zepbound) might help. Hashimoto's thyroiditis is an autoimmune condition causing hypothyroidism, affecting approximately 5% of Americans and frequently associated with weight gain and metabolic complications. While GLP-1 medications effectively treat type 2 diabetes and obesity, their role in Hashimoto's disease requires careful examination. This article reviews current evidence on GLP-1 use in patients with autoimmune thyroid disease, safety considerations, and appropriate treatment approaches.
Quick Answer: GLP-1 receptor agonists do not directly treat or improve Hashimoto's disease or its underlying autoimmune process, though they may be safely used for appropriate metabolic indications like type 2 diabetes or obesity in patients with this thyroid condition.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Hashimoto's disease, also known as Hashimoto's thyroiditis or chronic lymphocytic thyroiditis, is an autoimmune condition in which the immune system attacks the thyroid gland. This progressive destruction of thyroid tissue often leads to hypothyroidism—an underactive thyroid that cannot produce sufficient thyroid hormones to meet the body's needs. According to the American Thyroid Association, Hashimoto's disease is the most common cause of hypothyroidism in the United States, affecting approximately 5% of the general population and occurring more frequently in women than men.
The thyroid gland plays a crucial role in regulating metabolism, energy production, body temperature, and numerous other physiological processes. When thyroid function declines, patients commonly experience fatigue, weight gain, cold intolerance, constipation, dry skin, hair loss, and cognitive difficulties. The metabolic slowdown associated with hypothyroidism can make weight management particularly challenging, even with appropriate thyroid hormone replacement therapy.
Some studies suggest that individuals with Hashimoto's disease may develop metabolic complications beyond thyroid dysfunction itself. Research indicates associations between autoimmune thyroid disease and insulin resistance, metabolic syndrome, and type 2 diabetes, though these relationships vary by population and the degree of hypothyroidism. The relationship between thyroid function and metabolic health is bidirectional and complex—thyroid hormones influence glucose metabolism and insulin sensitivity, while metabolic dysfunction can affect thyroid hormone conversion and action at the cellular level.
This metabolic overlap has led some patients and clinicians to wonder whether medications targeting metabolic pathways, such as GLP-1 receptor agonists, might offer benefits for individuals with Hashimoto's disease. Understanding both conditions and their interconnections is essential for evaluating potential therapeutic approaches and managing patient expectations appropriately.
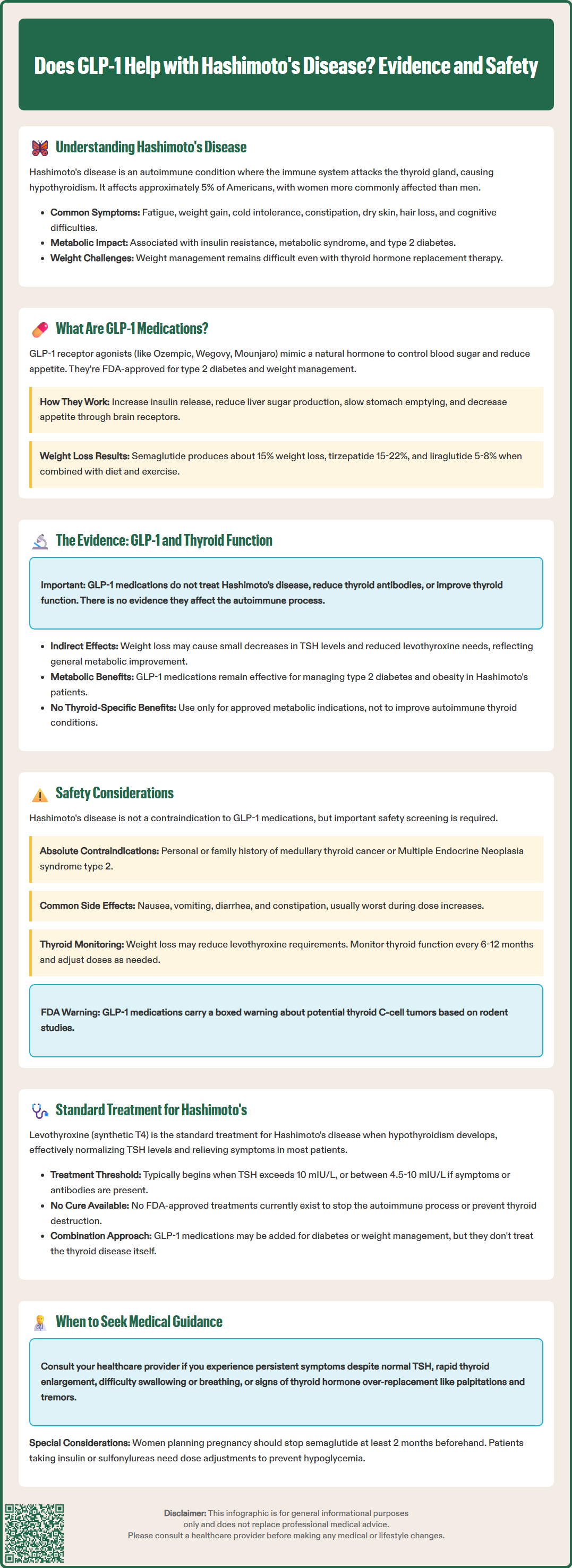
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed for type 2 diabetes management and subsequently approved for chronic weight management. These medications include semaglutide (Ozempic, Wegovy), liraglutide (Victoza, Saxenda), dulaglutide (Trulicity), tirzepatide (Mounjaro, Zepbound—which also targets GIP receptors), and several others. The FDA has approved various formulations for different indications based on clinical trial evidence.
GLP-1 is a naturally occurring incretin hormone released by intestinal cells in response to food intake. It plays multiple roles in glucose homeostasis and appetite regulation. GLP-1 receptor agonists mimic this endogenous hormone but are modified to resist rapid degradation, allowing for once-weekly or once-daily dosing depending on the specific medication. These agents work through several complementary mechanisms that improve metabolic control.
Primary mechanisms of action include:
Enhanced insulin secretion: GLP-1 receptor agonists stimulate glucose-dependent insulin release from pancreatic beta cells, meaning insulin secretion increases when blood glucose is elevated but not when glucose levels are normal or low, reducing hypoglycemia risk
Suppressed glucagon secretion: These medications inhibit glucagon release from pancreatic alpha cells, decreasing hepatic glucose production
Delayed gastric emptying: GLP-1 receptor activation slows the rate at which food leaves the stomach, moderating postprandial glucose excursions
Central appetite regulation: GLP-1 receptors in the brain, particularly in areas controlling satiety and food reward, are activated, leading to reduced appetite and caloric intake
These combined effects result in improved glycemic control in patients with type 2 diabetes and significant weight loss in both diabetic and non-diabetic individuals. The weight loss achieved varies by specific medication and dose: semaglutide 2.4 mg (Wegovy) produces approximately 15% weight loss, tirzepatide (Zepbound) up to 15-22%, and liraglutide 3 mg (Saxenda) about 5-8%. When used with insulin or sulfonylureas, these medications may increase hypoglycemia risk, requiring dose adjustments of those agents.
According to FDA labeling and American Diabetes Association guidelines, GLP-1 receptor agonists are indicated for type 2 diabetes (as an adjunct to diet and exercise) and for chronic weight management in adults with BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related comorbidity. However, these medications do not directly target thyroid function or autoimmune processes, which is an important distinction when considering their potential role in Hashimoto's disease management.
There is currently no established evidence that GLP-1 receptor agonists directly treat or improve Hashimoto's disease or its underlying autoimmune pathology. While some GLP-1 receptors have been identified in human thyroid tissue (primarily in C-cells), the clinical significance of this finding remains unclear and limited. No research demonstrates that GLP-1 medications reduce thyroid antibody levels, slow autoimmune thyroid destruction, or improve thyroid function in patients with Hashimoto's disease.
The primary connection between GLP-1 medications and thyroid considerations relates to a specific safety concern rather than therapeutic benefit. Preclinical studies in rodents showed that GLP-1 receptor agonists, particularly at high doses, were associated with thyroid C-cell tumors (medullary thyroid carcinoma). While this finding has not been confirmed in humans during extensive clinical trials and post-marketing surveillance, the FDA requires a boxed warning on GLP-1 receptor agonist labels regarding this potential risk. These medications are contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
Some observational data suggest that weight loss achieved through any means—including GLP-1 medications, bariatric surgery, or lifestyle modification—may have modest effects on thyroid function tests in individuals with obesity. Weight reduction can sometimes lead to small decreases in TSH levels and may reduce levothyroxine requirements in some patients with hypothyroidism. However, these changes reflect metabolic improvements associated with weight loss rather than any direct effect on the autoimmune process or thyroid gland itself.
Research examining metabolic benefits of GLP-1 receptor agonists in patients with coexisting type 2 diabetes and autoimmune thyroid disease has shown that these medications remain effective for glycemic control and weight management in this population. However, no studies demonstrate improvement in thyroid-specific outcomes such as antibody titers, thyroid hormone levels, or disease progression. Patients with Hashimoto's disease who have metabolic indications for GLP-1 therapy (type 2 diabetes or obesity) may benefit from these medications for those specific conditions, but should not expect direct thyroid benefits.
For patients with Hashimoto's disease considering GLP-1 receptor agonist therapy for appropriate metabolic indications, several safety considerations warrant careful attention. The most important distinction is between Hashimoto's thyroiditis (an autoimmune condition causing hypothyroidism) and medullary thyroid carcinoma (a rare thyroid cancer arising from C-cells), as these represent entirely different thyroid pathologies with different implications for GLP-1 use.
Hashimoto's disease itself is not a contraindication to GLP-1 receptor agonist use. Patients with autoimmune hypothyroidism who have appropriate indications—such as type 2 diabetes or obesity with weight-related comorbidities—may safely use these medications under medical supervision. However, the boxed warning regarding thyroid C-cell tumors observed in rodent studies remains relevant, and thorough patient screening is essential before initiating therapy.
Absolute contraindications to GLP-1 receptor agonists include:
Personal history of medullary thyroid carcinoma
Family history of medullary thyroid carcinoma
Multiple Endocrine Neoplasia syndrome type 2 (MEN 2)
Pregnancy (for weight management indications)
Severe gastrointestinal disease, including gastroparesis
Patients should be specifically questioned about these conditions during pre-treatment evaluation. For patients planning pregnancy, semaglutide should be discontinued at least 2 months before a planned pregnancy due to its long half-life. Routine measurement of serum calcitonin (a marker for C-cell pathology) is not recommended by most guidelines, as its value for screening in the general population is limited by poor specificity and the rarity of medullary thyroid carcinoma.
Common adverse effects of GLP-1 receptor agonists—including nausea, vomiting, diarrhea, and constipation—occur with similar frequency in patients with and without thyroid disease. These gastrointestinal symptoms are typically most pronounced during dose escalation and often improve with continued use. More serious but rare adverse effects include pancreatitis, gallbladder disease (cholelithiasis, cholecystitis), and acute kidney injury, which require prompt medical evaluation if symptoms develop. Patients should seek immediate care for right upper quadrant pain, fever, or jaundice.
Patients with diabetes using insulin or sulfonylureas with GLP-1 agents have an increased risk of hypoglycemia and may need dose adjustments of these medications. Those with diabetic retinopathy should have appropriate ophthalmologic monitoring when starting semaglutide, as rapid improvement in glucose control may temporarily worsen retinopathy.
Patients with Hashimoto's disease taking levothyroxine should be aware that significant weight loss from any cause may affect thyroid hormone requirements. Thyroid function tests should be monitored periodically (typically every 6-12 months or when symptoms suggest over- or under-replacement), and levothyroxine doses adjusted accordingly. Weight loss may reduce levothyroxine requirements in some individuals, though this is not universal. Any symptoms suggesting thyroid hormone imbalance—such as new or worsening fatigue, palpitations, heat or cold intolerance, or changes in weight beyond expected GLP-1 effects—should prompt thyroid function testing and clinical reassessment.
The standard and evidence-based treatment for Hashimoto's disease remains levothyroxine (synthetic T4) replacement therapy when hypothyroidism develops. Levothyroxine effectively replaces deficient thyroid hormone, normalizes TSH levels, and alleviates symptoms of hypothyroidism in the vast majority of patients. According to American Thyroid Association guidelines, treatment is typically initiated when TSH rises above 10 mIU/L or when TSH is between 4.5-10 mIU/L with symptoms or positive thyroid antibodies. Dosing is individualized based on body weight, age, and clinical response, with typical starting doses of 1.6 mcg/kg/day in younger adults. For older adults or those with coronary artery disease, lower starting doses with gradual titration are recommended.
During pregnancy, TSH targets are lower (typically <2.5 mIU/L in the first trimester), and treatment may be initiated at lower TSH thresholds. More frequent monitoring and dose adjustments are often needed during pregnancy.
There is currently no FDA-approved treatment that targets the underlying autoimmune process in Hashimoto's disease or prevents progression of thyroid destruction. While some complementary approaches—including selenium supplementation, dietary modifications, and stress reduction—have been studied, evidence for their efficacy remains limited and inconsistent. Patients should discuss any complementary therapies with their healthcare provider to ensure safety and avoid interactions with conventional treatment.
For patients with Hashimoto's disease who also have obesity or type 2 diabetes, a comprehensive treatment approach addressing all conditions is appropriate. GLP-1 receptor agonists may be considered for their FDA-approved indications—glycemic control in type 2 diabetes or chronic weight management in obesity—but should not be viewed as treatments for Hashimoto's disease itself. The decision to use these medications should be based on metabolic indications, patient preferences, contraindications, and cost considerations.
Patients should seek medical evaluation if they experience:
Persistent symptoms despite adequate levothyroxine replacement (confirmed by normal TSH)
Rapid thyroid enlargement or development of thyroid nodules
Difficulty swallowing or breathing related to thyroid enlargement
Symptoms suggesting thyroid hormone over-replacement (palpitations, tremor, anxiety, heat intolerance)
Regular monitoring of thyroid function is essential for patients with Hashimoto's disease. TSH should be checked 6-8 weeks after initiating or adjusting levothyroxine, then annually once stable levels are achieved. More frequent monitoring may be needed during pregnancy, with significant weight changes, or when medications affecting thyroid hormone metabolism are started or stopped. Patients considering GLP-1 therapy should inform their endocrinologist or primary care provider, as thyroid function monitoring may need to be intensified during periods of significant weight loss. A collaborative approach involving endocrinology, primary care, and when appropriate, nutrition and mental health support, provides optimal outcomes for patients managing both thyroid and metabolic conditions.
No, there is no evidence that GLP-1 receptor agonists reduce thyroid antibodies, improve thyroid function, or slow the autoimmune destruction of the thyroid gland in Hashimoto's disease. These medications do not target autoimmune pathology.
Yes, Hashimoto's disease itself is not a contraindication to GLP-1 use. Patients with autoimmune hypothyroidism who have appropriate indications such as type 2 diabetes or obesity may safely use these medications under medical supervision, provided they do not have a personal or family history of medullary thyroid carcinoma or MEN 2 syndrome.
Significant weight loss from GLP-1 therapy may reduce levothyroxine requirements in some patients. Thyroid function tests should be monitored periodically during treatment, and levothyroxine doses adjusted as needed based on TSH levels and clinical symptoms.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.