LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Semaglutide, marketed as Ozempic for type 2 diabetes and Wegovy for weight management, has raised questions about its effects on testosterone levels. This GLP-1 receptor agonist works by enhancing insulin secretion, suppressing appetite, and promoting significant weight loss. While concerns exist about hormonal impacts, current evidence does not support that semaglutide directly lowers testosterone. In fact, the substantial weight loss achieved with semaglutide may actually increase testosterone levels in men with obesity, while beneficially reducing elevated androgens in women with polycystic ovary syndrome. Understanding the distinction between direct drug effects and metabolic consequences is essential for patients and clinicians.
Quick Answer: Semaglutide does not directly lower testosterone levels and may actually increase testosterone in men with obesity through weight loss-related metabolic improvements.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (under the brand name Ozempic), chronic weight management (Wegovy), and cardiovascular risk reduction in adults with established cardiovascular disease and obesity or overweight. This medication works by mimicking the naturally occurring GLP-1 hormone, which enhances insulin secretion in response to meals, suppresses glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways.
The endocrine system operates through complex interconnected pathways, and medications affecting one hormone can potentially influence others. Testosterone, the primary androgen hormone, plays crucial roles in both men and women, including maintaining muscle mass, bone density, libido, mood regulation, and metabolic function. In men, testosterone is produced primarily in the testes, while women produce smaller amounts in the ovaries and adrenal glands.
GLP-1 receptors are found throughout the body, including in pancreatic beta cells, the gastrointestinal tract, brain, and cardiovascular tissues. While the evidence regarding GLP-1 receptor expression in testosterone-producing tissues is limited and mixed in humans, the metabolic changes induced by semaglutide—particularly significant weight loss and improved insulin sensitivity—can indirectly affect hormone balance. Understanding this distinction between potential direct pharmacological effects and indirect metabolic consequences is essential when evaluating semaglutide's impact on testosterone levels.
Patients and clinicians often question whether semaglutide directly suppresses testosterone production or whether any hormonal changes result from the medication's intended metabolic effects, particularly substantial weight reduction.
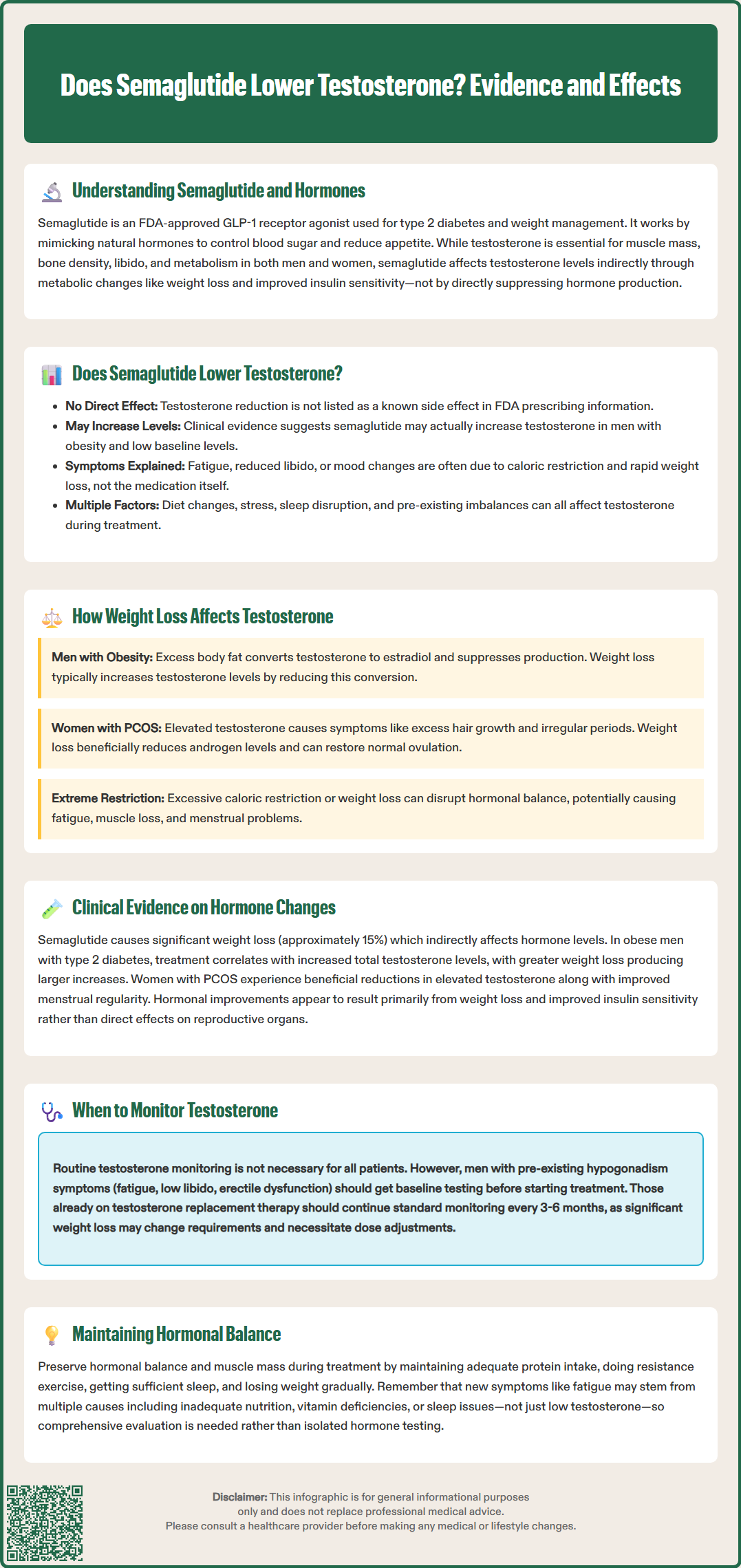
There is no established direct mechanism by which semaglutide lowers testosterone levels. The FDA-approved prescribing information for both Ozempic and Wegovy does not list testosterone reduction as a known adverse effect, and the medication does not act on androgen receptors or directly inhibit testosterone synthesis pathways. Current evidence suggests that semaglutide does not pharmacologically suppress testosterone production through its GLP-1 receptor agonist activity.
In fact, emerging clinical data indicates that semaglutide may be associated with increased testosterone levels in certain populations, particularly in men with obesity and low baseline testosterone. This apparent paradox—concerns about testosterone reduction versus evidence of testosterone elevation—reflects the complex relationship between body weight, metabolic health, and hormonal balance rather than a direct drug effect on testosterone production.
The confusion surrounding this topic often stems from individual patient experiences and the multifactorial nature of testosterone regulation. Factors such as caloric restriction, rapid weight loss, changes in body composition, stress, sleep disruption, and concurrent medical conditions can all influence testosterone levels during treatment. When patients experience symptoms potentially attributable to low testosterone—such as fatigue, reduced libido, or mood changes—while taking semaglutide, it may be tempting to attribute these symptoms directly to the medication.
However, these symptoms can also result from the caloric deficit associated with significant weight loss, adjustment to dietary changes, or pre-existing hormonal imbalances that become more apparent during metabolic transition. Distinguishing between medication effects, weight loss consequences, and coincidental hormonal changes requires careful clinical evaluation and appropriate laboratory testing.
The relationship between body weight and testosterone differs substantially between men and women, and understanding these sex-specific patterns is crucial when interpreting hormonal changes during semaglutide therapy. In men with obesity, excess adipose tissue contains aromatase enzyme, which converts testosterone to estradiol, effectively reducing circulating testosterone levels. Additionally, obesity is associated with insulin resistance, chronic inflammation, and hypothalamic-pituitary-gonadal axis dysfunction, all of which can suppress testosterone production.
Clinical studies consistently demonstrate that weight loss in men with obesity typically increases total testosterone levels. This improvement occurs through multiple mechanisms: reduced aromatase activity as fat mass decreases, improved insulin sensitivity, decreased inflammatory cytokines, and restoration of normal hypothalamic-pituitary function. Weight loss also typically increases sex hormone-binding globulin (SHBG) levels as insulin sensitivity improves, which affects the interpretation of total versus free testosterone measurements. Men with obesity-related hypogonadism often experience improvements in testosterone levels with sustained weight reduction, though the response varies between individuals and may require weight loss greater than 5-10% in some cases.
In women, the hormonal response to weight loss is more complex. Women with polycystic ovary syndrome (PCOS) and obesity often have elevated androgen levels, including testosterone, contributing to symptoms such as hirsutism, acne, and irregular menstruation. Weight loss in this population typically reduces testosterone and other androgen levels, which is therapeutically beneficial and can restore ovulatory function and improve metabolic parameters.
For women without PCOS, testosterone levels are naturally much lower than in men, and the impact of weight loss on testosterone is less pronounced and clinically significant. However, extreme caloric restriction or excessive weight loss can potentially disrupt hormonal balance in both sexes, potentially leading to relative energy deficiency in sport (RED-S) or hypothalamic dysfunction. This can contribute to fatigue, reduced muscle mass, menstrual irregularities in women, and decreased bone density. The rate and magnitude of weight loss, nutritional adequacy, and maintenance of lean body mass all influence hormonal outcomes during weight reduction therapy.
Several clinical trials and observational studies have examined metabolic changes associated with semaglutide treatment, though specific hormonal parameters including testosterone were not primary endpoints in most pivotal trials. The STEP (Semaglutide Treatment Effect in People with obesity) clinical trial program, which evaluated once-weekly semaglutide 2.4 mg for weight management, demonstrated significant weight loss (approximately 15% in STEP 1) that could indirectly affect hormone levels, though testosterone was not systematically reported in these publications.
Observational studies and smaller clinical trials have examined men with obesity and type 2 diabetes treated with GLP-1 receptor agonists, including semaglutide. Results from these studies suggest increases in total testosterone levels correlating with the degree of weight loss achieved. Men who lost more weight experienced greater testosterone elevation. These improvements were typically accompanied by increases in sex hormone-binding globulin (SHBG) due to improved insulin sensitivity, which affects the interpretation of total versus free testosterone measurements.
In women with PCOS and obesity, studies of GLP-1 receptor agonists have demonstrated reductions in elevated androgen levels, including testosterone, along with improvements in menstrual regularity and ovulation rates. These changes are considered beneficial in this population, as hyperandrogenism contributes to PCOS symptomatology and metabolic complications. The hormonal improvements appear to result primarily from weight loss and improved insulin sensitivity rather than proven direct effects on ovarian function.
Importantly, no large-scale clinical trials have identified clinically significant testosterone suppression as an adverse effect of semaglutide in either men or women without pre-existing hormonal disorders. FDA Adverse Event Reporting System (FAERS) data similarly do not suggest a pattern of treatment-emergent hypogonadism attributable to semaglutide. Individual case reports of hormonal changes during treatment should be interpreted in the context of multiple contributing factors, including baseline hormonal status, concurrent medications, rate of weight loss, nutritional intake, and other medical conditions.
Routine testosterone monitoring is not recommended for all patients taking semaglutide, as there is no evidence that the medication causes clinically significant testosterone suppression requiring systematic surveillance. However, specific clinical scenarios warrant baseline and follow-up testosterone assessment to ensure appropriate hormonal balance during treatment and to identify any underlying endocrine disorders that may require intervention.
Men with pre-existing symptoms suggestive of hypogonadism—including persistent fatigue, reduced libido, erectile dysfunction, decreased muscle mass, or depressed mood—should undergo testosterone evaluation before initiating semaglutide. According to American Urological Association guidelines, a total testosterone level below 300 ng/dL is considered low. Baseline testing should include total testosterone measured in the morning (between 7-11 AM when levels are highest), and if low, confirmatory repeat testing on a separate day along with luteinizing hormone (LH), follicle-stimulating hormone (FSH), and prolactin to characterize the type of hypogonadism. In men with obesity, assessment of free testosterone or bioavailable testosterone may be warranted when SHBG levels are abnormal. This baseline assessment helps distinguish pre-existing hormonal issues from any changes that might occur during treatment.
Patients who develop new symptoms potentially attributable to low testosterone during semaglutide therapy should be evaluated clinically and biochemically. However, clinicians should maintain a broad differential diagnosis, as symptoms such as fatigue and reduced libido can result from multiple causes, including inadequate caloric intake, nutrient deficiencies (particularly vitamin D, iron, or B vitamins), sleep disturbances, depression, or other medical conditions. A comprehensive metabolic panel, complete blood count, thyroid function tests, and vitamin levels may be more informative than isolated testosterone measurement in many cases.
For men with known hypogonadism receiving testosterone replacement therapy, monitoring should continue according to established guidelines from the American Urological Association and the Endocrine Society, typically every 3-6 months initially and then annually once stable. This should include hematocrit/hemoglobin and PSA (in appropriate age/risk groups). Significant weight loss may alter testosterone pharmacokinetics and requirements, potentially necessitating dose adjustments. Women with PCOS or hyperandrogenism may benefit from periodic androgen assessment to monitor therapeutic response, though this should be guided by clinical symptoms and treatment goals rather than arbitrary testing schedules.
Immediate endocrinology referral is warranted for patients with very low testosterone levels accompanied by normal or low LH/FSH, elevated prolactin, or symptoms such as headaches or visual disturbances that might suggest pituitary dysfunction.
Key monitoring recommendations include:
Baseline testosterone assessment for men with symptoms of hypogonadism before starting semaglutide
Evaluation of new or worsening symptoms during treatment with comprehensive metabolic and hormonal testing as clinically indicated
Continued monitoring for patients on testosterone replacement therapy according to standard guidelines
Consideration of nutritional status, sleep quality, and psychological factors when interpreting symptoms
Referral to endocrinology for complex cases or when hormonal abnormalities are identified
Patients should be counseled that significant weight loss itself typically improves testosterone levels in men with obesity and that any concerning symptoms should be reported promptly for appropriate evaluation. Maintaining adequate protein intake, engaging in resistance exercise, ensuring sufficient sleep, and achieving gradual rather than excessively rapid weight loss can help preserve hormonal balance and lean body mass during treatment.
No, semaglutide does not directly cause low testosterone. Clinical evidence suggests that weight loss from semaglutide typically increases testosterone levels in men with obesity by reducing fat tissue that converts testosterone to estrogen and improving metabolic function.
Routine testosterone monitoring is not necessary for all patients on semaglutide. However, men with pre-existing symptoms of low testosterone (fatigue, reduced libido, erectile dysfunction) should have baseline testing before starting treatment and follow-up if symptoms develop or worsen.
In women with polycystic ovary syndrome and elevated testosterone, semaglutide-related weight loss typically reduces androgen levels beneficially, improving symptoms like irregular periods and hirsutism. In women without PCOS, testosterone changes are minimal and not clinically significant.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.