LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide safe while breastfeeding remains an important question for lactating individuals managing type 2 diabetes or obesity. Tirzepatide (Mounjaro, Zepbound) is a dual GIP and GLP-1 receptor agonist approved by the FDA in 2022. Currently, no human data exist on tirzepatide transfer into breast milk or its effects on nursing infants. The FDA label explicitly states this knowledge gap, requiring healthcare providers and patients to make individualized decisions weighing maternal treatment needs against theoretical infant risks. Understanding available evidence and safer alternatives helps inform these critical decisions during the postpartum period.
Quick Answer: Tirzepatide safety during breastfeeding is unknown, as no human data exist on its transfer into breast milk or effects on nursing infants.
Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved for type 2 diabetes management and chronic weight management. As a relatively new medication approved by the FDA in 2022, limited data exist regarding its safety during breastfeeding.
The primary concern with any medication during lactation is whether it transfers into breast milk and, if so, whether it poses risks to the nursing infant. Tirzepatide is a large peptide molecule with a molecular weight of approximately 4,813 daltons. While larger molecules generally have reduced transfer into breast milk compared to smaller compounds, transfer can still occur and may vary in the early postpartum period when breast tissue permeability is higher. However, the extent of tirzepatide excretion in human milk remains unknown, as systematic studies in lactating individuals have not been conducted.
Animal studies provide limited insight. In lactating rats, tirzepatide was detected in milk, though the clinical significance of these findings for humans is uncertain due to physiological differences between species. The potential exposure to breastfed infants and any clinical significance cannot be determined without human data.
Currently, there is no official confirmation that tirzepatide is safe during breastfeeding. Healthcare providers must weigh the potential benefits of maternal treatment against theoretical risks to the infant, considering the importance of both diabetes control and breastfeeding for maternal and infant health.
The FDA-approved prescribing information for tirzepatide explicitly states that "there are no data on the presence of tirzepatide in human milk, the effects on the breastfed infant, or the effects on milk production." This absence of data reflects the exclusion of pregnant and breastfeeding individuals from clinical trials, a common practice that creates knowledge gaps for this population.
The FDA label advises that "the developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for tirzepatide and any potential adverse effects on the breastfed infant from tirzepatide or from the underlying maternal condition." This guidance places decision-making responsibility on the healthcare provider and patient, requiring individualized risk-benefit assessment.
Importantly, the FDA does not provide a specific recommendation to avoid or continue tirzepatide during lactation. Instead, it acknowledges the complexity of the decision. Factors to consider include the severity of maternal diabetes or obesity, availability of alternative treatments, the infant's age and health status, and whether breastfeeding is exclusive or supplemented with formula.
The American Diabetes Association (ADA) guidelines emphasize the importance of glycemic control during the postpartum period but do not specifically address tirzepatide use during breastfeeding due to insufficient evidence. Healthcare providers should document discussions about unknown risks and shared decision-making when considering tirzepatide in lactating patients.
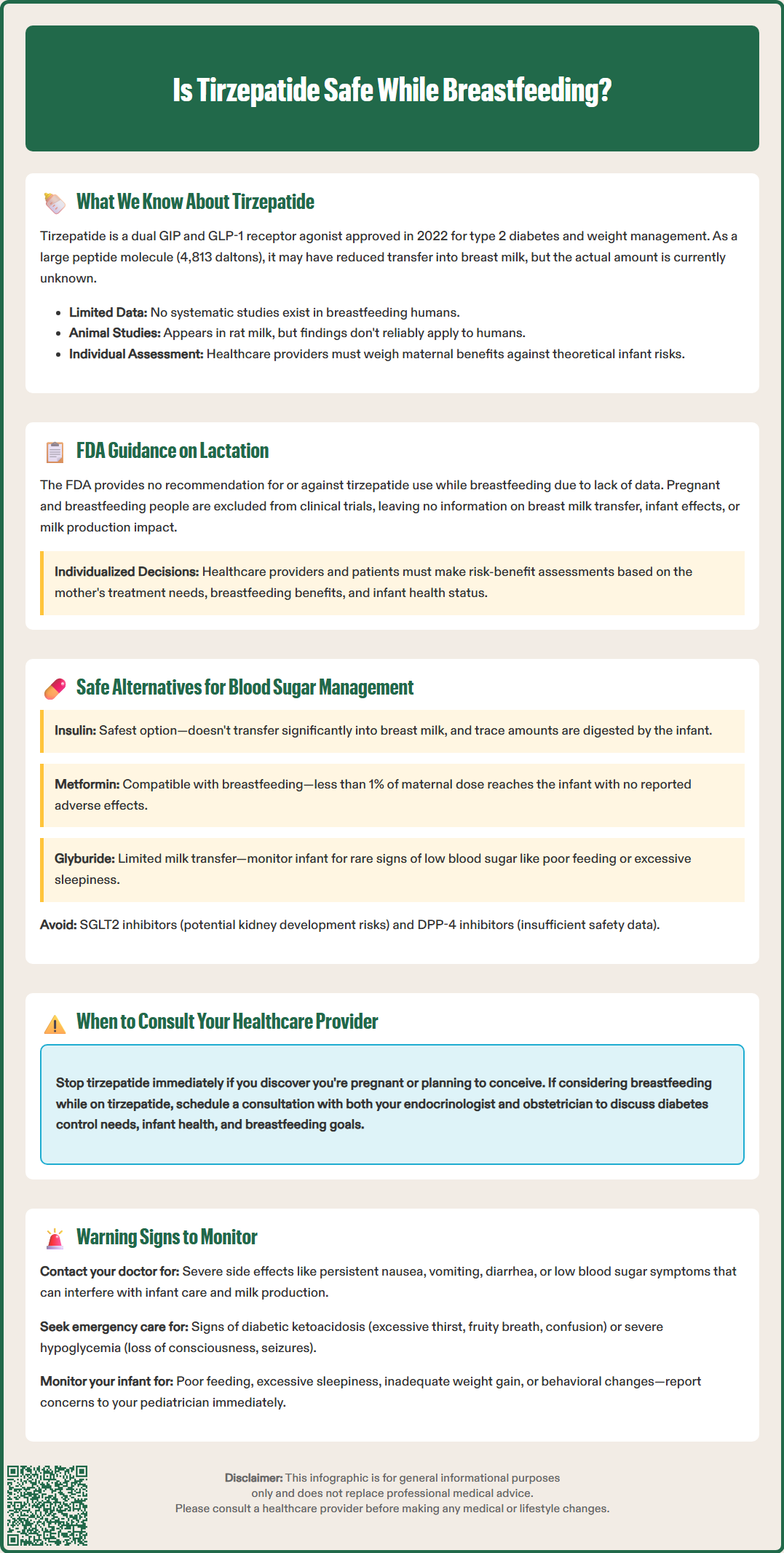
Several diabetes medications have established safety profiles during breastfeeding, making them preferred options for lactating individuals requiring pharmacological blood sugar management. Insulin remains the gold standard for diabetes treatment during lactation. As a large peptide hormone, insulin does not transfer significantly into breast milk, and any small amounts present would be digested in the infant's gastrointestinal tract. All insulin formulations—including rapid-acting, short-acting, intermediate-acting, and long-acting preparations—are considered compatible with breastfeeding.
Metformin, a first-line oral medication for type 2 diabetes, transfers into breast milk in minimal amounts. Multiple studies have demonstrated that infant exposure through breast milk is clinically insignificant, with no adverse effects reported. The NIH LactMed database and other professional organizations consider metformin compatible with breastfeeding. Typical maternal doses result in infant exposure of less than 1% of a weight-adjusted maternal dose.
Glyburide, a second-generation sulfonylurea, has limited transfer into breast milk and is considered acceptable during lactation, though insulin is generally preferred for better glycemic control. When using sulfonylureas, monitoring the infant for signs of hypoglycemia (poor feeding, excessive sleepiness) is advisable, though such effects are rare.
Some medications should be avoided during breastfeeding, including SGLT2 inhibitors, due to potential risks to infant renal development based on animal data. DPP-4 inhibitors have limited human lactation data.
Non-pharmacological approaches remain foundational for blood sugar management during lactation. These include:
Medical nutrition therapy with carbohydrate monitoring and portion control
Regular physical activity as tolerated postpartum
Continuous glucose monitoring to identify patterns and adjust treatment
Frequent self-monitoring of blood glucose to maintain target ranges
Lactation itself has metabolic benefits, as milk production requires approximately 330-400 additional calories daily in the early months and about 400 calories daily later in lactation. However, breastfeeding can also increase hypoglycemia risk in insulin-treated individuals, necessitating careful monitoring and potential medication adjustment.
Immediate consultation is warranted if you are currently taking tirzepatide and discover you are pregnant or plan to breastfeed. If you are planning pregnancy, discuss with your healthcare provider when to discontinue tirzepatide. While the FDA does not specify a required washout period before conception, tirzepatide has a half-life of approximately 5 days, and some clinicians may recommend discontinuation several weeks before attempting conception based on pharmacokinetic properties.
If you become pregnant while taking tirzepatide, contact your healthcare provider promptly to discuss alternative diabetes management strategies.
For individuals considering breastfeeding while taking tirzepatide, schedule a preconception or early postpartum consultation with both your endocrinologist and obstetrician. This discussion should address:
Your specific diabetes control needs and whether alternative medications could provide adequate glycemic management
The infant's health status, as premature or medically fragile infants may warrant more conservative medication approaches
Your breastfeeding goals, including whether you plan exclusive breastfeeding or combination feeding
Monitoring strategies for both maternal blood sugar control and infant growth and development
Contact your healthcare provider if you experience severe or persistent side effects while taking any diabetes medication during lactation, including nausea, vomiting, diarrhea, or signs of hypoglycemia (shakiness, sweating, confusion). These symptoms can affect your ability to care for your infant and maintain adequate nutrition for milk production.
Seek urgent medical attention if you develop signs of diabetic ketoacidosis (excessive thirst, frequent urination, fruity breath odor, confusion) or severe hypoglycemia (loss of consciousness, seizures). Additionally, consult your pediatrician if your breastfed infant shows unusual symptoms such as poor feeding, excessive sleepiness, inadequate weight gain, or any concerning changes in behavior or development. Since human milk transfer of tirzepatide is unknown, monitoring the infant is important if maternal treatment is necessary.
A multidisciplinary approach involving endocrinology, obstetrics, and pediatrics ensures comprehensive care that prioritizes both maternal health and infant safety during this critical period.
It is unknown whether tirzepatide passes into human breast milk, as no studies have been conducted in lactating individuals. Animal studies detected tirzepatide in rat milk, but the relevance to humans remains uncertain.
Insulin and metformin are considered safe during breastfeeding with established evidence. Insulin does not transfer significantly into breast milk, and metformin transfers in clinically insignificant amounts with no reported adverse infant effects.
Consult your healthcare provider before breastfeeding while taking tirzepatide. Due to lack of safety data, your provider may recommend switching to medications with established lactation safety profiles such as insulin or metformin.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.