LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Does tirzepatide make you tired? While fatigue is not among the most common side effects reported in clinical trials, some patients experience tiredness during treatment with this dual GIP and GLP-1 receptor agonist. Tirzepatide, approved by the FDA as Mounjaro for type 2 diabetes and Zepbound for chronic weight management, primarily causes gastrointestinal side effects. However, indirect mechanisms—including reduced caloric intake from appetite suppression, gastrointestinal symptoms affecting nutrition, and metabolic changes from weight loss—may contribute to feelings of fatigue. Understanding these potential causes and management strategies can help patients optimize their treatment experience while maintaining therapeutic benefits.
Quick Answer: Tirzepatide may cause tiredness in some patients, though fatigue is not listed among the most common side effects in clinical trials, with indirect mechanisms like reduced caloric intake and gastrointestinal effects potentially contributing to this symptom.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). While fatigue is not listed among the most common adverse effects in the Mounjaro prescribing information, it is reported by some patients during treatment.
In clinical trials for type 2 diabetes, fatigue was not identified as a frequent side effect occurring in more than 5% of participants. The most commonly reported adverse reactions include gastrointestinal symptoms such as nausea, diarrhea, vomiting, constipation, and abdominal discomfort. However, patient experiences suggest that some individuals may experience fatigue during treatment.
Several indirect mechanisms may contribute to feelings of fatigue in patients taking tirzepatide. These include reduced caloric intake due to appetite suppression, gastrointestinal side effects leading to decreased food intake, delayed gastric emptying, changes in blood glucose levels, and the metabolic adjustments associated with significant weight loss. It is important to distinguish between medication-related fatigue and tiredness resulting from lifestyle changes, underlying medical conditions, or other medications.
Importantly, tirzepatide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
Patients experiencing persistent or severe fatigue while taking tirzepatide should consult their healthcare provider for proper evaluation. Fatigue may indicate other medical issues requiring investigation, such as anemia, thyroid dysfunction, vitamin deficiencies, or inadequate glycemic control. Seek immediate medical attention for severe abdominal pain, persistent vomiting, signs of dehydration, or allergic reactions.
Understanding the potential mechanisms behind fatigue during tirzepatide therapy requires consideration of both the medication's pharmacological effects and the physiological changes it induces. Tirzepatide works by activating GIP and GLP-1 receptors, which enhance insulin secretion in a glucose-dependent manner, suppress glucagon release, slow gastric emptying, and reduce appetite through central nervous system pathways.
The significant appetite suppression caused by tirzepatide often leads to reduced caloric intake, which is therapeutic for weight loss but may result in insufficient energy consumption for some patients. When caloric intake drops substantially, particularly if protein intake is inadequate, patients may experience fatigue, weakness, and reduced physical stamina. This energy deficit, while contributing to weight loss, can manifest as tiredness, especially during the initial weeks of treatment or following dose escalations.
Gastrointestinal side effects, particularly nausea and vomiting, may further compromise nutritional status by limiting food intake. Persistent vomiting could potentially lead to dehydration and electrolyte imbalances, which can cause fatigue and reduced energy levels. The delayed gastric emptying effect of tirzepatide may also contribute to feelings of fullness and reduced food intake.
Changes in blood glucose patterns may also play a role. While tirzepatide improves overall glycemic control in patients with type 2 diabetes, some individuals may experience hypoglycemia (blood glucose <70 mg/dL), particularly if they are also taking insulin or sulfonylureas. Hypoglycemia can cause fatigue, weakness, and confusion. Furthermore, the metabolic changes accompanying significant weight loss—including alterations in hormone levels, body composition, and energy expenditure—may temporarily affect energy levels as the body adapts to a new physiological state.
Other common contributors to fatigue should also be considered, including sleep apnea (common in obesity), depression, anemia, and thyroid dysfunction. Patients taking metformin along with tirzepatide may be at increased risk for vitamin B12 deficiency, which can cause fatigue.
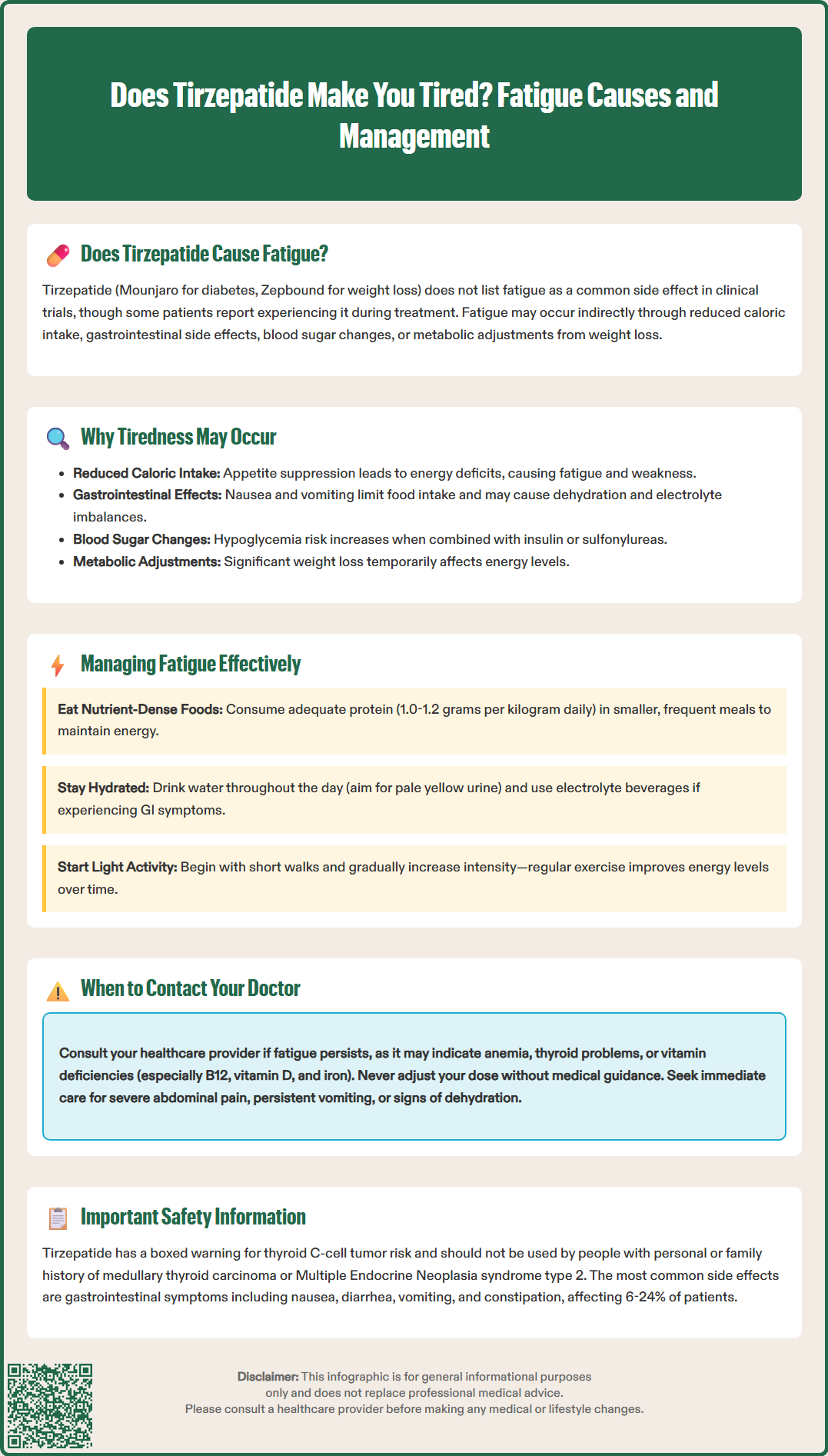
If you experience fatigue while taking tirzepatide, several practical strategies may help manage this symptom while continuing treatment. First, ensure adequate nutritional intake despite reduced appetite. Focus on nutrient-dense foods that provide essential vitamins, minerals, and macronutrients in smaller volumes. Prioritize high-quality protein sources (lean meats, fish, eggs, legumes) to preserve muscle mass during weight loss, aiming for 1.0 to 1.2 grams of protein per kilogram of body weight daily during active weight loss, as tolerated and appropriate for your kidney function.
Maintain proper hydration by drinking adequate fluids throughout the day, particularly if experiencing gastrointestinal side effects. Dehydration can significantly contribute to fatigue and is often overlooked. Monitor your hydration status by checking that your urine is pale yellow in color. Consider electrolyte-containing beverages if experiencing vomiting or diarrhea.
Monitor your eating patterns and consider smaller, more frequent meals rather than three large meals daily. This approach may help manage nausea while ensuring consistent energy intake. Avoid skipping meals, as this can exacerbate fatigue and potentially lead to hypoglycemia in patients with diabetes. Keep healthy snacks readily available, such as nuts, Greek yogurt, or protein bars.
Gradual physical activity can paradoxically improve energy levels despite initial fatigue. Start with light exercise such as short walks and gradually increase intensity as tolerated. Regular physical activity improves cardiovascular fitness, enhances mood, and can help combat fatigue over time. However, listen to your body and avoid overexertion, especially during the initial treatment period.
If side effects are severe, your healthcare provider may recommend temporarily holding your dose or slowing the titration schedule. Never adjust your dose without medical guidance. Seek immediate medical attention if you experience severe abdominal pain, inability to keep fluids down for more than 24 hours, signs of dehydration, or allergic reactions.
Consult your healthcare provider if fatigue persists or worsens. They may recommend laboratory testing to evaluate for anemia, thyroid dysfunction, vitamin deficiencies (particularly B12 if you also take metformin, vitamin D, and iron), or other metabolic abnormalities. In some cases, supplementation may be appropriate. Your provider may also review your medication regimen to identify potential drug interactions or consider adjusting the tirzepatide dose if side effects are limiting tolerability.
Beyond potential fatigue, tirzepatide is associated with several well-documented side effects, predominantly affecting the gastrointestinal system. Understanding these adverse effects helps patients recognize expected symptoms and identify situations requiring medical attention.
Important Safety Information: Tirzepatide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Patients should be counseled about thyroid tumor symptoms (neck mass, dysphagia, dyspnea, persistent hoarseness).
Gastrointestinal effects are the most frequently reported side effects and include:
Nausea (12–24% of patients): Often most pronounced during treatment initiation and dose escalation, typically improving over time
Diarrhea (13–23% of patients): May be transient or persistent, requiring dietary modifications
Vomiting (6–11% of patients): Can lead to dehydration if severe or prolonged
Constipation (6–17% of patients): May require increased fiber intake and hydration
Abdominal pain or discomfort (6–10% of patients): Usually mild to moderate in severity
Decreased appetite: Therapeutic effect but may be excessive in some individuals
These gastrointestinal symptoms generally diminish over several weeks as the body adjusts to the medication. Gradual dose titration, as recommended in the prescribing information, helps minimize these effects. Tirzepatide is not recommended for patients with severe gastrointestinal disease, including severe gastroparesis.
Hypoglycemia risk is low when tirzepatide is used as monotherapy but increases when combined with insulin or sulfonylureas. Patients taking these combinations require careful glucose monitoring and may need dose reductions of insulin or sulfonylureas when starting tirzepatide. Symptoms of hypoglycemia include shakiness, sweating, confusion, and dizziness.
Injection site reactions, including redness, itching, or swelling, occur in approximately 2–3% of patients. These are typically mild and resolve spontaneously. Rotating injection sites can help minimize local reactions.
Hair loss (alopecia) has been reported in clinical trials for weight management.
Serious but rare adverse effects require immediate medical attention and include:
Pancreatitis: Severe abdominal pain radiating to the back, with or without vomiting
Gallbladder disease: Right upper quadrant pain, particularly after meals
Acute kidney injury: Usually secondary to severe dehydration from gastrointestinal symptoms
Severe allergic reactions: Rash, difficulty breathing, or swelling of face, lips, or throat
Patients should contact their healthcare provider if they experience persistent vomiting, severe abdominal pain, signs of dehydration, or any concerning symptoms. Regular monitoring and patient education regarding potential adverse effects are recommended when initiating therapy with tirzepatide.
Fatigue was not identified as a frequent side effect in clinical trials, occurring in less than 5% of participants. The most common side effects are gastrointestinal symptoms such as nausea, diarrhea, and vomiting, though some patients do report tiredness during treatment.
Tiredness may result from reduced caloric intake due to appetite suppression, gastrointestinal side effects limiting food consumption, dehydration from vomiting or diarrhea, changes in blood glucose levels, or metabolic adjustments during significant weight loss. These indirect mechanisms can affect energy levels during treatment.
Contact your healthcare provider if fatigue is persistent, severe, or worsening, as it may indicate underlying issues such as anemia, thyroid dysfunction, vitamin deficiencies, or inadequate glycemic control. Seek immediate medical attention for severe abdominal pain, persistent vomiting, signs of dehydration, or allergic reactions.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.