LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
How to know if tirzepatide is working involves monitoring specific clinical markers and physical changes that indicate the medication is exerting its therapeutic effects. Tirzepatide, a dual GIP and GLP-1 receptor agonist approved for type 2 diabetes and chronic weight management, produces measurable improvements in appetite, metabolic parameters, and body weight over time. Recognizing these signs—from early appetite suppression to sustained reductions in blood glucose and body weight—helps patients and clinicians assess treatment efficacy and make informed decisions about dose optimization and ongoing management.
Quick Answer: Tirzepatide is working when you experience reduced appetite within 1-4 weeks, measurable weight loss by 4-8 weeks, and improved blood glucose levels (for diabetes patients) within 2-4 weeks of treatment initiation.
Tirzepatide is a glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (under the brand name Mounjaro) and chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity (under the brand name Zepbound). For weight management, tirzepatide must be used in conjunction with a reduced-calorie diet and increased physical activity.
The pharmacological mechanism of tirzepatide involves simultaneous activation of both GIP and GLP-1 receptors, which are incretin hormones naturally released by the intestine in response to food intake. By activating GLP-1 receptors, tirzepatide enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriately elevated glucagon secretion, and slows gastric emptying. The additional GIP receptor activation may further enhance insulin secretion and appears to contribute to the medication's effects on weight reduction.
Tirzepatide also acts centrally to reduce appetite and food intake by affecting areas of the brain involved in appetite regulation. The medication is administered once weekly via subcutaneous injection, with doses typically initiated at 2.5 mg (an initiation dose not intended for glycemic control) and gradually titrated upward (5 mg, 7.5 mg, 10 mg, 12.5 mg, to a maximum of 15 mg) based on glycemic response, weight loss goals, and tolerability. This gradual dose escalation helps minimize gastrointestinal adverse effects.
Important safety information: Tirzepatide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2). It should not be used in patients with severe gastroparesis. Patients taking insulin or insulin secretagogues (such as sulfonylureas) may have an increased risk of hypoglycemia and may require dose adjustments of these medications. Tirzepatide may reduce the effectiveness of oral contraceptives, particularly during dose initiation and escalation periods.
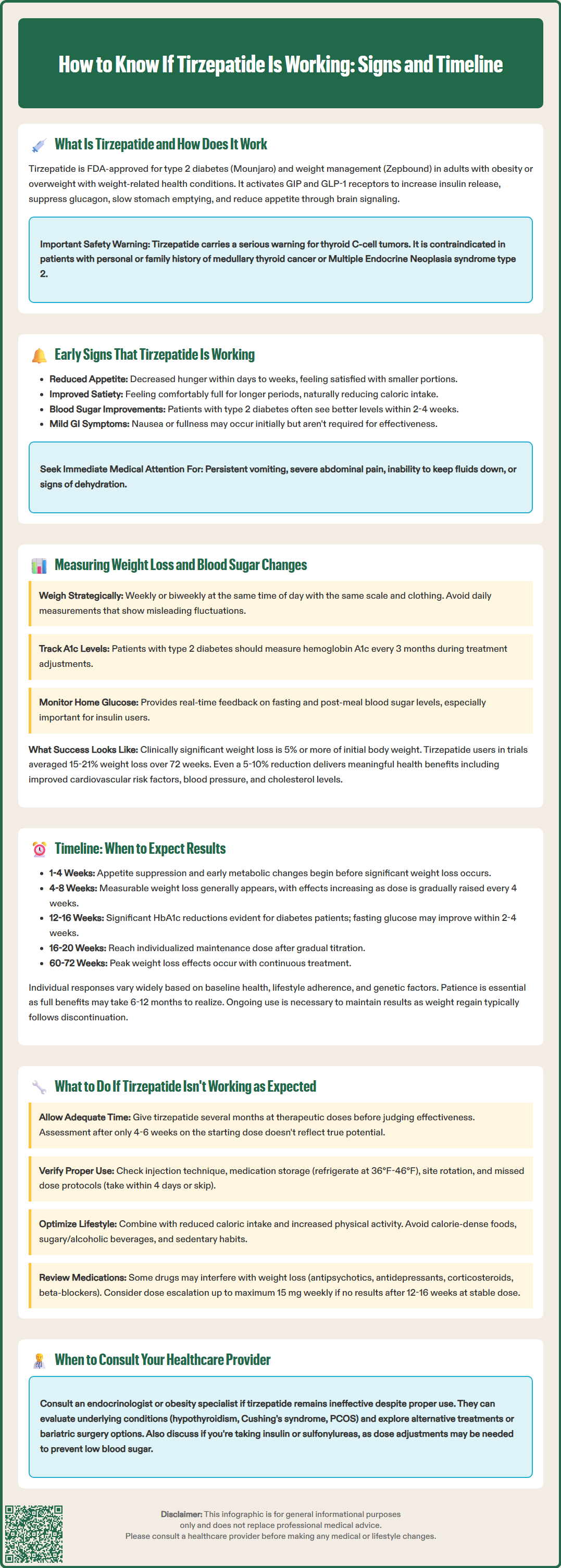
Patients often notice several early indicators that tirzepatide is beginning to exert its therapeutic effects, typically within the first few weeks of treatment. The most commonly reported early sign is reduced appetite and decreased hunger, which many patients experience within days to weeks of starting therapy. This appetite suppression often manifests as feeling satisfied with smaller portion sizes, reduced cravings for high-calorie foods, and less frequent thoughts about eating between meals. These changes reflect tirzepatide's effects on central appetite regulation and delayed gastric emptying.
Improved satiety and prolonged fullness after meals is another early indicator of medication efficacy. Patients frequently report feeling comfortably full for longer periods following meals, which naturally leads to reduced caloric intake without the sensation of deprivation or active restriction. Some individuals may also notice changes in food preferences, though this effect varies considerably among patients and is based primarily on anecdotal reports.
Gastrointestinal symptoms may occur during the initial weeks, particularly following dose increases. While mild nausea, occasional changes in bowel habits, or a sense of fullness are common, these symptoms are not necessary for the medication to be effective. Importantly, patients should contact their healthcare provider immediately if they experience severe or persistent gastrointestinal symptoms, severe abdominal pain (which could indicate pancreatitis or gallbladder disease), persistent vomiting, inability to keep fluids down, or signs of dehydration.
For patients with type 2 diabetes who monitor their blood glucose levels at home, early improvements in fasting and postprandial glucose readings may be observed within the first 2–4 weeks of treatment. These changes often precede significant weight loss. Patients taking insulin or sulfonylureas should monitor blood glucose more frequently and work with their healthcare provider to adjust these medications as needed to prevent hypoglycemia.
Objective measurement of tirzepatide's effectiveness requires systematic tracking of both weight and metabolic parameters. Weight should be measured consistently—ideally at the same time of day, using the same scale, and wearing similar clothing—to minimize variability. Weekly or biweekly weigh-ins are generally recommended rather than daily measurements, as day-to-day fluctuations due to fluid shifts, dietary sodium intake, and hormonal changes can obscure the underlying trend. Recording weight in a log or smartphone application allows patients and clinicians to identify patterns and calculate the rate of weight loss over time.
Clinically significant weight loss is typically defined as a reduction of 5% or more of initial body weight, though many patients on tirzepatide achieve greater reductions. In clinical trials of adults without diabetes (SURMOUNT-1), patients treated with tirzepatide for chronic weight management lost an average of 15–21% of their body weight over 72 weeks, depending on the dose used. Weight loss in patients with type 2 diabetes is typically lower but still significant. A weight loss of 5–10% still confers meaningful health benefits, including improvements in cardiovascular risk factors, blood pressure, and lipid profiles.
For patients with type 2 diabetes, hemoglobin A1c (HbA1c) measurement provides the most reliable assessment of glycemic control over the preceding 2–3 months. The American Diabetes Association recommends checking HbA1c every 3 months when therapy is adjusted or when glycemic targets are not being met, and at least twice yearly in patients meeting treatment goals. Tirzepatide has demonstrated robust HbA1c reductions in clinical trials, with mean decreases ranging from 1.9% to 2.4% from baseline, depending on dose and baseline values.
Home glucose monitoring offers additional real-time feedback, particularly for patients on insulin or other glucose-lowering medications that may require adjustment as tirzepatide takes effect. Fasting glucose levels and pre-meal readings provide insight into basal glucose control, while postprandial measurements (taken 1–2 hours after meals) reflect the medication's effects on meal-related glucose excursions. Continuous glucose monitoring (CGM) may be particularly helpful for patients at risk of hypoglycemia. Patients should discuss target glucose ranges with their healthcare provider, as these vary based on individual circumstances, comorbidities, and hypoglycemia risk.
Understanding the expected timeline for tirzepatide's effects helps set realistic expectations and allows for appropriate clinical assessment. Appetite suppression and early metabolic changes typically emerge within the first 1–4 weeks of treatment, though the magnitude of these effects often increases with dose escalation. Patients may notice reduced hunger, improved satiety, and initial changes in eating patterns during this early phase, even before substantial weight loss occurs.
Measurable weight loss generally becomes apparent within 4–8 weeks of initiating tirzepatide, with the rate of loss typically accelerating as the dose is titrated upward according to the prescribing protocol. The FDA-approved dosing schedule involves increasing the dose every 4 weeks, which means patients progressively experience greater pharmacological effects over the first several months of treatment. Most patients do not reach their maintenance dose until 16–20 weeks after initiation, and weight loss continues throughout this titration period and beyond. The maintenance dose is individualized based on response and tolerability; not all patients require escalation to the maximum 15 mg dose.
Glycemic improvements in patients with type 2 diabetes often precede maximal weight loss effects. Fasting glucose levels may begin to decline within 2–4 weeks, with more substantial HbA1c reductions becoming evident at 12–16 weeks (the typical interval for HbA1c reassessment). In the SURPASS clinical trials, significant HbA1c reductions were observed by 40 weeks, though individual patients may achieve glycemic targets earlier, particularly at higher doses.
Peak weight loss effects in clinical trials were typically observed between 60–72 weeks of continuous treatment, with some variation between patients with obesity (SURMOUNT trials) and those with type 2 diabetes (SURPASS trials). After reaching a weight plateau, continued treatment is generally necessary to maintain weight loss, as discontinuation often results in weight regain. The American Medical Association, American Association of Clinical Endocrinology, and other professional organizations recognize obesity as a chronic disease requiring long-term management, and tirzepatide is intended for ongoing use rather than short-term intervention.
It is important to note that individual responses vary based on baseline weight, metabolic health, adherence to lifestyle modifications, concurrent medications, and genetic factors. Some patients experience rapid early responses, while others demonstrate a more gradual trajectory. Patience during the initial months of treatment is essential, as the full therapeutic potential of tirzepatide may not be realized until 6–12 months of treatment.
When tirzepatide appears to be producing suboptimal results, a systematic evaluation is warranted before concluding that the medication is ineffective. First, verify that adequate time has elapsed for the medication to exert its full effects. As noted, meaningful weight loss and glycemic improvements may require several months, particularly if dose titration is still ongoing. Premature assessment—such as evaluating efficacy after only 4–6 weeks on the initial 2.5 mg dose—may not reflect the medication's true potential at therapeutic doses.
Ensure proper injection technique and medication storage, as these factors can affect drug delivery and stability. Tirzepatide should be stored in the refrigerator (36°F to 46°F) until use, though it may be kept at room temperature (up to 86°F) for up to 21 days if needed. The medication should be injected subcutaneously into the abdomen, thigh, or upper arm, rotating injection sites to prevent lipohypertrophy. If a dose is missed, it should be administered within 4 days of the scheduled dose; if more than 4 days have passed, skip the missed dose and administer the next dose on the regularly scheduled day.
Assess adherence to lifestyle modifications, as tirzepatide is most effective when combined with reduced caloric intake and increased physical activity. While the medication significantly reduces appetite, patients who continue to consume calorie-dense foods or maintain sedentary habits may experience attenuated weight loss. A frank discussion about dietary patterns, portion sizes, beverage choices (particularly sugar-sweetened or alcoholic drinks), and physical activity levels can identify modifiable factors that may be limiting treatment response.
Review concurrent medications that may interfere with weight loss or glycemic control. Certain medications—including some antipsychotics, antidepressants, corticosteroids, and beta-blockers—can promote weight gain or worsen insulin resistance. While these medications should not be discontinued without medical guidance, discussing alternatives with the prescribing physician may be appropriate in some cases.
Consider dose optimization. If a patient has been on a stable dose for 12–16 weeks without achieving expected results, and tolerability permits, advancing to the next dose level may enhance efficacy. The maximum approved dose is 15 mg weekly for both diabetes and weight management indications. Generally, reassessment after approximately 3 months at a maintenance dose is appropriate, and alternative strategies may be considered if less than 5% weight loss has been achieved.
If tirzepatide remains ineffective despite adequate dosing, duration, and adherence, further evaluation for secondary causes of obesity or poor glycemic control may be indicated. Conditions such as hypothyroidism, Cushing's syndrome, polycystic ovary syndrome, or medication-induced weight gain should be considered. Additionally, some patients may have genetic or metabolic factors that limit their response to incretin-based therapies.
Consultation with an endocrinologist or obesity medicine specialist is appropriate when first-line management with tirzepatide does not produce expected results. These specialists can provide comprehensive evaluation, consider alternative or adjunctive pharmacological options, and discuss other interventions such as intensive lifestyle programs or bariatric surgery for patients with severe obesity (typically BMI ≥35 kg/m² with comorbidities or ≥40 kg/m² without) who do not respond adequately to medical management. Patients should be reassured that lack of response to one medication does not preclude success with alternative approaches.
Importantly, patients should immediately contact their healthcare provider if they experience severe abdominal pain (which could indicate pancreatitis), persistent vomiting, inability to keep fluids down, signs of dehydration, or allergic reactions. Women of childbearing potential should be advised that tirzepatide may reduce the effectiveness of oral contraceptives, particularly during dose initiation and escalation periods, and should consider using non-oral or additional contraceptive methods.
Most patients notice reduced appetite within 1-4 weeks of starting tirzepatide, with measurable weight loss typically becoming apparent within 4-8 weeks. Peak weight loss effects are generally observed between 60-72 weeks of continuous treatment, as the dose is gradually titrated upward.
Patients with type 2 diabetes typically see fasting glucose levels begin to decline within 2-4 weeks of starting tirzepatide. HbA1c reductions of 1.9-2.4% are commonly observed when measured at 12-16 weeks, though individual responses vary based on baseline values and dose.
If tirzepatide appears ineffective, first ensure adequate time has elapsed (at least 3 months at a maintenance dose) and verify proper injection technique, medication storage, and adherence to lifestyle modifications. Discuss dose optimization with your healthcare provider, and consider consultation with an endocrinologist or obesity medicine specialist if results remain suboptimal despite appropriate dosing and duration.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.