LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Starting tirzepatide for the first time involves a structured approach designed to optimize safety and effectiveness. Tirzepatide is a dual GIP and GLP-1 receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound) in adults with obesity or overweight with weight-related comorbidities. First-time users begin with a low 2.5 mg subcutaneous dose administered once weekly, primarily to establish tolerability. Understanding what to expect during initial weeks—including common gastrointestinal side effects, proper injection technique, and monitoring requirements—helps ensure successful treatment initiation and adherence to this evidence-based therapy.
Quick Answer: First-time tirzepatide users begin with a 2.5 mg subcutaneous injection once weekly, serving as a tolerability dose before gradual escalation every four weeks.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound) in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, as an adjunct to diet and physical activity.
When starting tirzepatide for the first time, patients typically begin with a low dose of 2.5 mg administered subcutaneously once weekly. This initial dose serves primarily as a tolerability step rather than a therapeutic dose, allowing your body to adjust to the medication's effects on glucose regulation and gastric emptying.
During the first four weeks, most patients notice gradual changes in appetite and satiety. Tirzepatide works by enhancing insulin secretion in a glucose-dependent manner, suppressing glucagon release, and slowing gastric emptying. These mechanisms contribute to improved glycemic control and reduced caloric intake. Many patients report feeling fuller sooner during meals and experiencing decreased food cravings between meals.
The medication follows a structured dose-escalation protocol, with increases every four weeks as tolerated. After the initial 2.5 mg dose, your healthcare provider will typically increase to 5 mg, then potentially to 7.5 mg, 10 mg, 12.5 mg, or the maximum dose of 15 mg, depending on your therapeutic goals and tolerability. This gradual titration minimizes gastrointestinal side effects while optimizing metabolic benefits.
It is important to understand that tirzepatide's full therapeutic effects develop over several weeks to months. Significant improvements in hemoglobin A1c typically become apparent after 12 weeks, while weight loss continues progressively over 6–12 months. Setting realistic expectations about this timeline helps maintain adherence during the initial adjustment period.
Important safety information: Tirzepatide has a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Report symptoms such as a lump in your neck, hoarseness, trouble swallowing, or shortness of breath to your healthcare provider immediately. Tirzepatide for weight management is not recommended during pregnancy, and you should discontinue if pregnancy occurs or is planned. The medication may reduce the effectiveness of oral contraceptives, particularly during initiation and dose increases, so use non-oral or barrier contraception for 4 weeks after starting and after each dose increase.
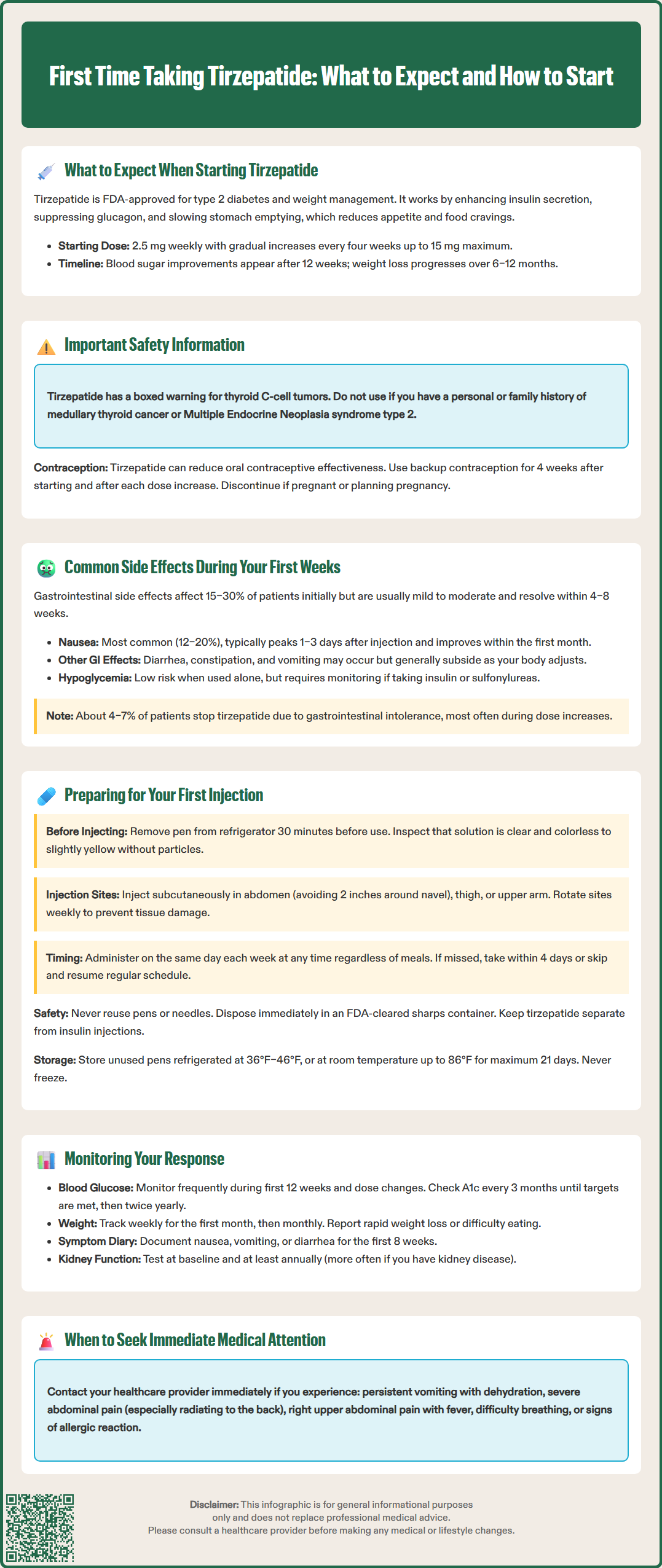
Gastrointestinal side effects are the most frequently reported adverse events when first taking tirzepatide, occurring in approximately 15–30% of patients during initial titration, with rates varying by dose and indication. These effects result from the medication's mechanism of slowing gastric emptying and are generally dose-dependent and transient. The most common gastrointestinal symptoms include:
Nausea (12–20% of patients): Usually mild to moderate, most pronounced 1–3 days after injection, typically improving within the first month
Diarrhea (7–16% of patients): Often resolves as the body adjusts to the medication
Decreased appetite: An expected pharmacologic effect that contributes to weight loss
Constipation (5–7% of patients): May require dietary fiber adjustments or stool softeners
Vomiting (2–8% of patients): Less common but warrants medical attention if persistent
Abdominal discomfort or bloating: Related to delayed gastric emptying
Most gastrointestinal side effects are mild to moderate in severity and diminish significantly after 4–8 weeks as tolerance develops. However, approximately 4–7% of patients discontinue tirzepatide due to gastrointestinal intolerance, most commonly during dose escalation phases.
Other potential side effects during the first weeks include injection site reactions (erythema, pruritus, or mild discomfort), fatigue, and headache. Hypoglycemia risk is generally low with tirzepatide monotherapy due to its glucose-dependent mechanism, but patients taking concurrent sulfonylureas or insulin require careful monitoring and possible dose adjustments of these medications.
When to seek medical attention: Contact your healthcare provider immediately if you experience:
Severe or persistent vomiting, signs of dehydration (dizziness, decreased urination)
Severe abdominal pain, especially if radiating to your back (may indicate pancreatitis)
Right upper abdominal pain, fever, or yellowing of skin/eyes (possible gallbladder disease)
Decreased urine output or swelling (potential kidney problems)
Neck mass, hoarseness, or difficulty swallowing (thyroid tumor warning signs)
Severe allergic reactions including swelling of face/lips/tongue or difficulty breathing
Visual changes (especially in patients with diabetic retinopathy)
Symptoms of hypoglycemia (if taking insulin or sulfonylureas)
Persistent nausea lasting beyond the first month or significantly impacting nutritional intake also warrants clinical evaluation.
Proper preparation for your first tirzepatide injection ensures safe administration and optimal therapeutic outcomes. Tirzepatide is supplied as single-dose prefilled pens in multiple strengths (2.5, 5, 7.5, 10, 12.5, and 15 mg), each containing 0.5 mL solution. Before your first injection, schedule time with your healthcare provider or diabetes educator for hands-on training in injection technique, as proper administration is essential for medication efficacy and safety.
Pre-injection preparation steps:
Remove the pen from refrigerated storage (36°F–46°F or 2°C–8°C) 30 minutes before injection to allow it to reach room temperature, which reduces injection discomfort
Inspect the solution through the pen window—it should be clear and colorless to slightly yellow; do not use if cloudy, discolored, or containing particles
Gather supplies: alcohol swab, sharps disposal container, and gauze if needed
Wash hands thoroughly with soap and water
Injection site selection and technique:
Tirzepatide is administered subcutaneously in the abdomen, thigh, or upper arm. Rotate injection sites weekly to prevent lipodystrophy. The abdomen should be avoided within 2 inches of the navel. Clean the selected site with an alcohol swab and allow to air dry completely.
Follow the manufacturer's Instructions for Use (IFU) specific to your pen (Mounjaro or Zepbound) for detailed steps on cap removal, pen activation, and proper injection technique. After injection, dispose of the pen immediately in an FDA-cleared sharps container—never reuse pens or needles.
If you are also using insulin, administer tirzepatide and insulin as separate injections at different sites; never mix them in the same syringe.
Timing and storage considerations: Tirzepatide can be administered at any time of day, with or without meals. Choose a consistent day each week (e.g., every Monday) to maintain steady medication levels. If a dose is missed, administer within 4 days; if more than 4 days have passed, skip the missed dose and resume your regular schedule.
Store unused pens in the refrigerator (36°F–46°F or 2°C–8°C). If needed, pens may be kept at room temperature (up to 86°F or 30°C) for up to 21 days. Protect from light, do not freeze, and discard if frozen.
Systematic monitoring during the first months of tirzepatide therapy allows for timely dose adjustments and identification of potential adverse effects. Your healthcare provider will establish a monitoring schedule tailored to your individual clinical situation, but general recommendations include specific metabolic, safety, and tolerability assessments.
Glycemic monitoring: For patients with type 2 diabetes, self-monitoring of blood glucose (SMBG) is particularly important during the first 12 weeks and during dose escalations. Patients taking concurrent insulin or sulfonylureas should monitor more frequently due to hypoglycemia risk. Hemoglobin A1c should be measured at baseline and approximately every 3 months until glycemic targets are achieved, then at least twice yearly. Clinical trials show that many patients achieve significant A1c reductions over time, with mean reductions of approximately 1.5–2.3% observed in pivotal trials at 40–52 weeks.
Weight and body composition: Regular weight monitoring (weekly during the first month, then monthly) helps assess therapeutic response and guides dose titration decisions. Document weight changes and discuss patterns with your healthcare provider. Report rapid, unintentional weight loss, signs of dehydration, or inability to maintain adequate nutrition, as these may require medical evaluation or nutritional counseling.
Safety monitoring parameters:
Gastrointestinal tolerance: Keep a symptom diary during the first 8 weeks, noting severity and duration of nausea, vomiting, or diarrhea
Hydration status: Monitor for signs of dehydration, especially if experiencing gastrointestinal side effects
Abdominal symptoms: Report persistent or severe abdominal pain promptly for evaluation of potential pancreatitis or gallbladder disease
Renal function: Assess at baseline and periodically per ADA guidelines (at least annually; more frequently if you have chronic kidney disease or are at risk for acute kidney injury)
Heart rate: Tirzepatide may cause modest heart rate increases (2–4 beats per minute); report palpitations or persistent tachycardia
Additional monitoring considerations:
If you have diabetic retinopathy, follow appropriate ophthalmology care as recommended by the ADA
If using tirzepatide for weight management, use non-oral contraception or backup contraceptive methods for 4 weeks after initiation and after each dose increase
Contact your healthcare provider immediately if pregnancy occurs or is planned, as tirzepatide for weight management is not recommended during pregnancy
Clinical follow-up schedule: Expect appointments at 4 weeks (first dose escalation), 8–12 weeks (metabolic assessment), and then every 3 months during the first year. Between appointments, contact your healthcare provider for severe or persistent side effects, inadequate glycemic control, or questions about dose adjustments.
The starting dose is 2.5 mg administered subcutaneously once weekly for four weeks. This initial dose serves primarily as a tolerability step, allowing your body to adjust before dose escalation to 5 mg and potentially higher doses based on therapeutic goals and side effect tolerance.
Significant improvements in hemoglobin A1c typically become apparent after 12 weeks of treatment. Full therapeutic effects develop over several weeks to months, with progressive changes continuing over 6–12 months as doses are titrated.
The most common side effects are gastrointestinal, including nausea (12–20% of patients), diarrhea (7–16%), decreased appetite, and constipation (5–7%). These effects are typically mild to moderate, most pronounced during the first 1–3 days after injection, and generally improve within 4–8 weeks as tolerance develops.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.