LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Weight loss plateaus during tirzepatide treatment are a common challenge that can be frustrating for patients who initially experienced significant progress. Tirzepatide, a dual GIP and GLP-1 receptor agonist approved by the FDA for type 2 diabetes (Mounjaro) and chronic weight management (Zepbound), typically produces substantial weight reduction, but this progress naturally slows over time. Understanding why stalls occur and implementing evidence-based strategies can help restart weight loss. This article explores the physiological reasons behind plateaus, identifies common contributing factors, and provides practical, medically sound approaches to overcome treatment stalls while maintaining realistic expectations for long-term success.
Quick Answer: Breaking a tirzepatide stall requires systematic dietary reassessment, increased physical activity, dose optimization with your physician, and addressing sleep and stress factors.
A weight loss plateau during tirzepatide therapy is a common phenomenon where weight reduction slows significantly or stops despite continued medication adherence. Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound) in adults with BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related comorbidity.
Clinical trials demonstrate that most patients experience substantial weight loss during treatment, with average reductions of 15-21% of initial body weight at maximum doses by approximately 72 weeks, as shown in the SURMOUNT-1 trial. This weight loss is not immediate or linear.
Plateaus typically occur after an initial period of consistent weight loss and represent a normal physiological adaptation rather than treatment failure. The body's metabolic rate adjusts to lower body weight through multiple mechanisms, including reduced energy expenditure, hormonal changes affecting appetite regulation, and alterations in fat oxidation. Weight loss plateaus lasting several weeks are not uncommon during pharmacotherapy for obesity.
Understanding that plateaus differ from treatment non-response is essential. A true plateau occurs after documented weight loss, whereas primary non-response indicates insufficient initial weight reduction. US guidelines typically recommend reassessing response after approximately 3 months at a maintenance dose, with ≥5% weight loss considered clinically meaningful. The SURMOUNT clinical trial program showed that weight loss velocity naturally decreases over time, even among responders, as patients approach what some researchers theorize as an individual metabolic set point. Recognizing this pattern helps maintain realistic expectations and prevents premature discontinuation of effective therapy.
Multiple factors contribute to weight loss plateaus during tirzepatide treatment, often involving complex interactions between medication effects, behavioral patterns, and physiological adaptations. Metabolic adaptation represents a primary biological cause, as the body reduces resting energy expenditure following significant weight loss. This adaptive thermogenesis occurs partly independently of changes in body composition and can partially counteract the caloric deficit created by reduced food intake, though the magnitude varies between individuals.
Dietary compensation frequently undermines continued weight loss. While tirzepatide effectively reduces appetite through central and peripheral mechanisms, patients may unconsciously increase portion sizes, caloric density of foods, or eating frequency as initial gastrointestinal side effects diminish. Research suggests that people often underestimate their caloric intake, particularly with calorie-dense foods like nuts, oils, processed snacks, and liquid calories including alcohol. Additionally, social eating situations and emotional eating patterns may re-emerge after the initial treatment phase.
Insufficient dose escalation can limit therapeutic effect. The FDA-approved titration schedule for tirzepatide involves gradual increases of 2.5 mg every four weeks, but some patients remain on suboptimal doses due to side effect concerns or insurance restrictions. Clinical data demonstrate dose-dependent weight loss, with maximum efficacy typically achieved at 10–15 mg weekly doses.
Other contributing factors include medication interactions (certain psychiatric medications, corticosteroids, and reduced exposure to oral contraceptives during dose escalation), hormonal changes (thyroid dysfunction, menopause), inadequate sleep (less than 7 hours nightly), chronic stress with elevated cortisol, and reduced physical activity as patients become more comfortable at their current weight. Medical conditions such as polycystic ovary syndrome (PCOS), Cushing's syndrome, or hypothyroidism may also impede progress and warrant evaluation if suspected.
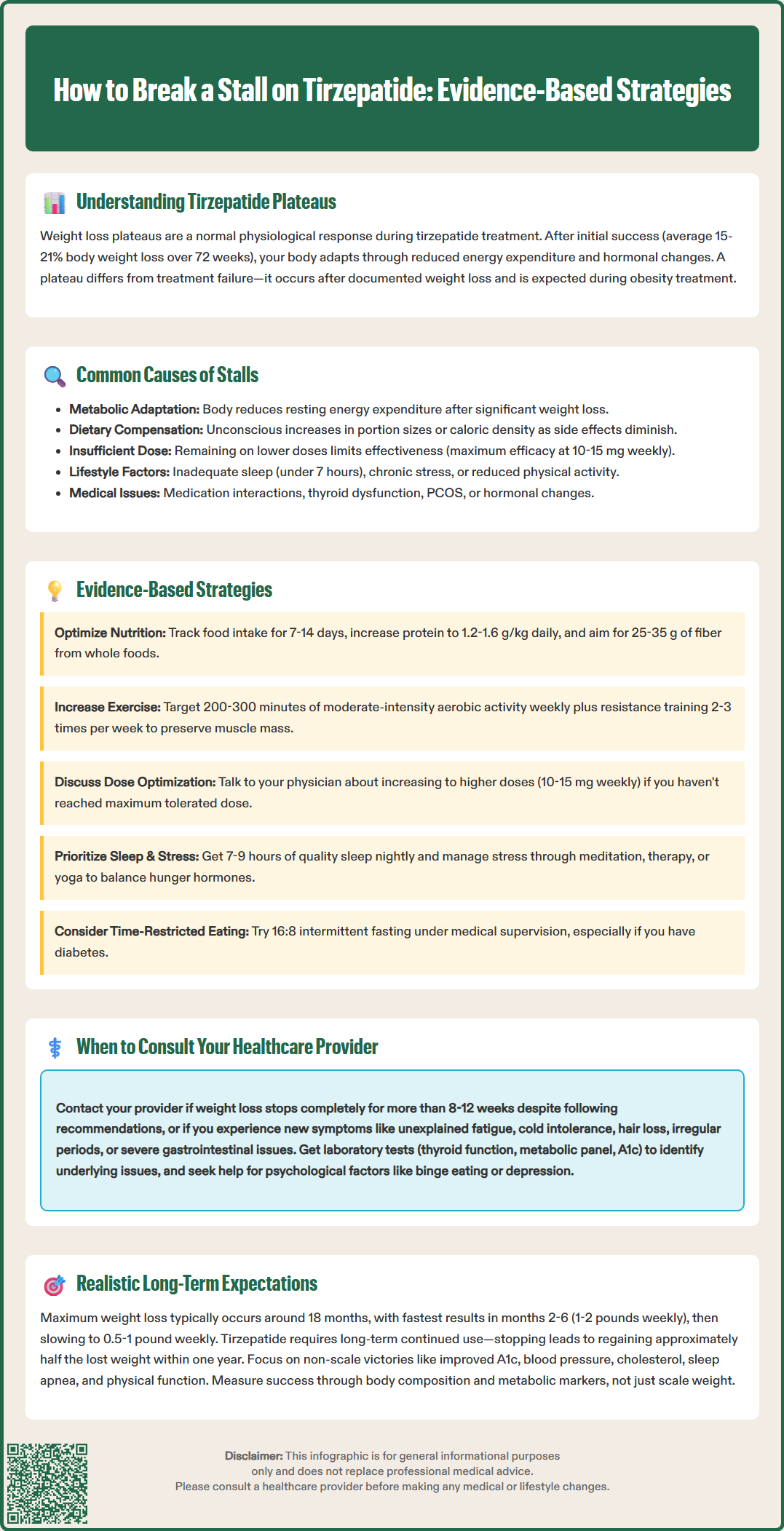
Breaking through a weight loss plateau requires a systematic, evidence-based approach addressing multiple factors simultaneously. Dietary reassessment forms the foundation of plateau management. Patients should track food intake meticulously for 7–14 days using validated apps or food diaries, focusing on portion sizes, cooking methods, and hidden calories in beverages and condiments. Consultation with a registered dietitian can identify areas for improvement, such as increasing protein intake to 1.2–1.6 g/kg of ideal body weight daily to preserve lean muscle mass and enhance satiety (with caution in chronic kidney disease; consult a healthcare provider if eGFR <60 mL/min). Reducing ultra-processed foods and emphasizing whole foods with high fiber content (25–35 g daily) improves glycemic control and promotes sustained fullness.
Physical activity modification plays a crucial role in overcoming metabolic adaptation. The American College of Sports Medicine recommends 200–300 minutes of moderate-intensity aerobic exercise weekly for weight loss maintenance, significantly more than the 150 minutes suggested for general health. Incorporating resistance training 2–3 times weekly helps preserve muscle mass, which maintains metabolic rate during weight loss. High-intensity interval training (HIIT) may provide additional metabolic benefits, though patients should consult their healthcare provider before initiating vigorous exercise programs.
Dose optimization should be discussed with the prescribing physician if the patient has not reached the maximum tolerated or FDA-approved dose. Clinical trials demonstrate continued weight loss with dose escalation, and many patients benefit from titration to 10 mg or 15 mg weekly if tolerability permits. However, dose increases should follow the FDA-recommended schedule of 2.5 mg increments every four weeks to minimize gastrointestinal adverse effects.
Addressing sleep quality and stress management provides often-overlooked benefits. Aim for 7–9 hours of quality sleep nightly, as sleep deprivation increases ghrelin (hunger hormone) and decreases leptin (satiety hormone). Stress reduction techniques such as mindfulness meditation, cognitive behavioral therapy, or yoga can lower cortisol levels that promote central adiposity. Some patients benefit from intermittent fasting approaches, such as time-restricted eating (16:8 protocol), though this should be implemented cautiously and under medical supervision, particularly in patients with diabetes using insulin or sulfonylureas due to hypoglycemia risk.
Certain circumstances warrant prompt medical evaluation rather than self-directed plateau management strategies. Patients should contact their healthcare provider if weight loss completely stops for more than 8–12 weeks despite documented adherence to medication, dietary modifications, and exercise recommendations. This duration helps distinguish normal fluctuations from potential treatment resistance or underlying medical issues requiring investigation.
New or worsening symptoms accompanying the plateau necessitate medical assessment. These include unexplained fatigue, cold intolerance, hair loss, or constipation (suggesting hypothyroidism); easy bruising, facial fullness, or purple striae (indicating possible Cushing's syndrome); or irregular menstrual cycles with hirsutism (raising concern for PCOS). Additionally, patients experiencing severe or persistent gastrointestinal side effects—including nausea, vomiting, diarrhea, or abdominal pain—should not attempt to self-manage these symptoms, as they may indicate pancreatitis, gallbladder disease (right upper quadrant pain, fever, jaundice), or other serious adverse effects requiring immediate evaluation. Signs of dehydration or acute kidney injury also warrant prompt attention.
Consultation is also appropriate when considering medication adjustments or additions. Healthcare providers can assess whether dose escalation is appropriate, evaluate potential drug interactions, or consider adjunctive therapies. Some patients may benefit from combination approaches, though adding other weight loss medications to tirzepatide has not been studied in clinical trials and should only occur under close supervision by specialists in obesity medicine. The provider can also order relevant laboratory investigations, including thyroid function tests (TSH, free T4), comprehensive metabolic panel, hemoglobin A1c, lipid profile, and pregnancy testing when appropriate to identify metabolic barriers to continued weight loss.
Psychological factors such as depression, binge eating disorder, or significant anxiety about weight may require referral to mental health specialists or eating disorder programs. The provider can facilitate appropriate referrals and ensure integrated care. Finally, if weight regain occurs (typically defined as regaining more than 3–5% of lost weight), prompt consultation allows for early intervention before significant regain undermines previous progress.
Establishing realistic expectations for tirzepatide therapy is essential for long-term success and patient satisfaction. Clinical trial data from the SURMOUNT-1 study demonstrated that patients achieved maximum weight loss at approximately 72 weeks (18 months), with average reductions of 15.0% (5 mg), 19.5% (10 mg), and 20.9% (15 mg) of initial body weight. However, individual responses vary considerably, with some patients losing more than 25% and others experiencing more modest reductions. Factors influencing individual response include baseline body mass index (BMI), insulin resistance severity, genetic factors, adherence patterns, and lifestyle modifications.
Weight loss velocity naturally decreases over time, following a logarithmic rather than linear pattern. The most rapid weight loss typically occurs during months 2–6 of therapy, with progressively slower rates thereafter. The CDC and clinical guidelines suggest that expecting 1–2 pounds weekly during the initial phase and 0.5–1 pound weekly during later phases represents a reasonable framework, though week-to-week fluctuations due to fluid retention, menstrual cycles, or dietary sodium intake are normal and should not cause alarm.
Long-term maintenance requires continued medication in most cases. The SURMOUNT-4 withdrawal trial showed that patients regain approximately half of lost weight within one year of stopping tirzepatide, highlighting that obesity is a chronic disease requiring ongoing management rather than a condition cured by temporary treatment. The American Diabetes Association Standards of Care and other professional guidelines recognize anti-obesity medications as long-term therapies, similar to medications for hypertension or diabetes.
Patients should understand that non-scale victories often prove more meaningful than numbers alone. Improvements in hemoglobin A1c, blood pressure, lipid profiles, sleep apnea severity, joint pain, and physical function represent significant health benefits even if weight loss plateaus. Quality of life enhancements, including improved mobility, self-confidence, and ability to participate in desired activities, constitute important treatment outcomes. Focusing exclusively on scale weight can lead to frustration and premature treatment discontinuation despite achieving substantial health improvements. Regular monitoring of body composition, waist circumference, and metabolic parameters provides a more comprehensive assessment of treatment success than weight alone.
Weight loss plateaus on tirzepatide can last several weeks and represent normal physiological adaptation. If weight loss completely stops for more than 8-12 weeks despite medication adherence and lifestyle modifications, consult your healthcare provider to evaluate potential underlying causes.
Dose optimization should only be discussed with your prescribing physician. If you have not reached the maximum tolerated or FDA-approved dose, your provider may recommend titration following the FDA schedule of 2.5 mg increments every four weeks to minimize side effects while potentially enhancing weight loss.
Track food intake meticulously for 7-14 days to identify hidden calories, increase protein to 1.2-1.6 g/kg ideal body weight daily, consume 25-35 g fiber daily, reduce ultra-processed foods, and consider consulting a registered dietitian. These evidence-based dietary modifications can help overcome metabolic adaptation and restart weight loss.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.