LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
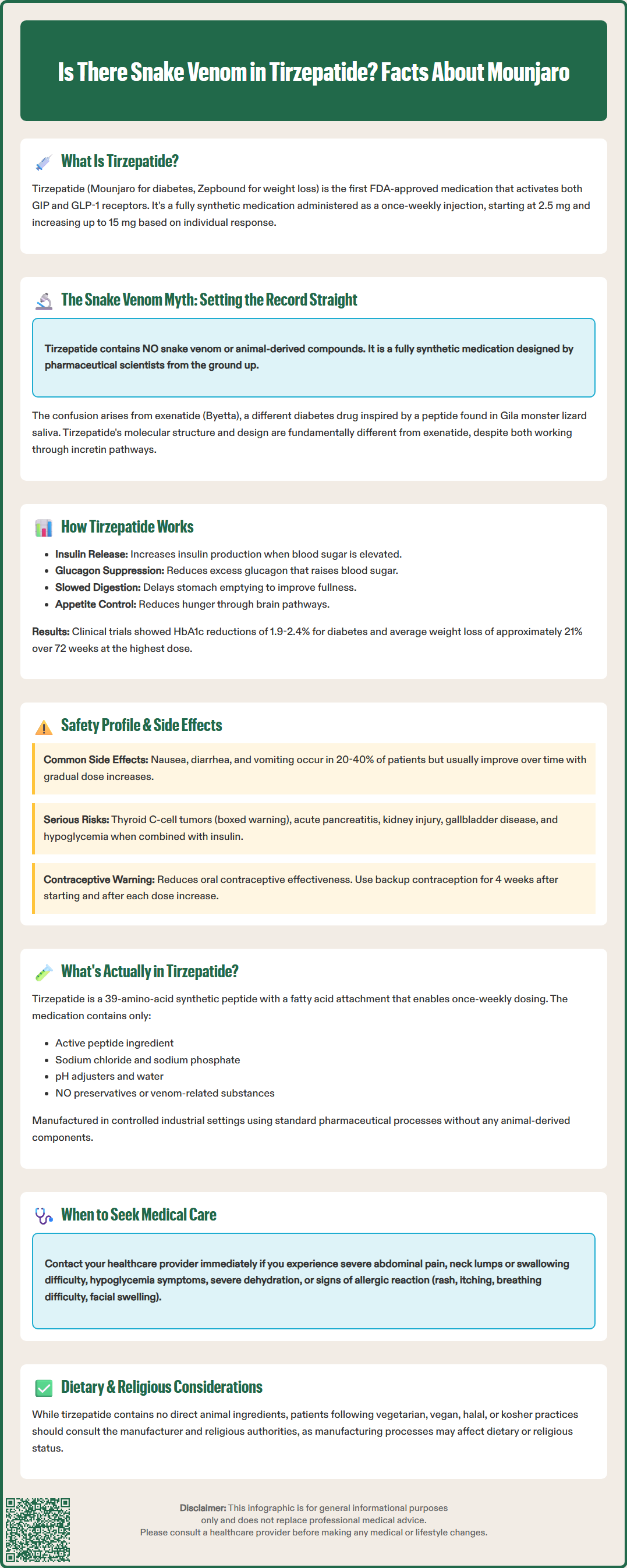
Is there snake venom in tirzepatide? This common question arises from confusion with earlier diabetes medications. Tirzepatide (Mounjaro, Zepbound) is a fully synthetic peptide medication approved by the FDA for type 2 diabetes and chronic weight management. Unlike exenatide, which was inspired by Gila monster venom, tirzepatide contains no animal-derived compounds or venom components. Understanding the true origins and composition of tirzepatide helps patients make informed decisions about this dual GIP/GLP-1 receptor agonist therapy.
Quick Answer: Tirzepatide contains no snake venom or animal-derived compounds; it is an entirely synthetic peptide medication designed and manufactured in pharmaceutical laboratories.
Tirzepatide is a synthetic peptide medication approved by the FDA for the treatment of type 2 diabetes mellitus (marketed as Mounjaro) and chronic weight management (marketed as Zepbound). It represents a novel therapeutic class as the first dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist.
The medication works through a dual mechanism of action that targets two incretin hormone pathways simultaneously. By activating GIP receptors, tirzepatide enhances insulin secretion and may improve insulin sensitivity in peripheral tissues. Concurrently, GLP-1 receptor activation stimulates glucose-dependent insulin release from pancreatic beta cells, suppresses inappropriate glucagon secretion, slows gastric emptying, and reduces appetite through central nervous system pathways. This combined approach results in improved glycemic control and significant weight reduction.
Tirzepatide is administered as a once-weekly subcutaneous injection, with dosing typically initiated at 2.5 mg and titrated upward based on therapeutic response and tolerability. The maximum approved dose is 15 mg weekly for diabetes management. In the SURPASS clinical trial program, tirzepatide demonstrated HbA1c reductions of 1.9% to 2.4% at the 15 mg dose, and in the SURPASS-2 trial specifically showed greater efficacy compared to semaglutide 1 mg. In the SURMOUNT-1 obesity trial, participants achieved weight loss averaging up to approximately 21% of baseline body weight at 72 weeks with the 15 mg dose.
It is important to understand that tirzepatide is entirely synthetic and not derived from any animal source. The molecular structure was designed by pharmaceutical scientists to optimize receptor binding and pharmacokinetic properties. Tirzepatide is not indicated for the treatment of type 1 diabetes.
The question about snake venom in tirzepatide stems from confusion with exenatide (Byetta, Bydureon), an earlier GLP-1 receptor agonist that does have origins in reptile biology. Exenatide's development was inspired by exendin-4, a peptide found in the saliva of the Gila monster (Heloderma suspectum), a venomous lizard native to the southwestern United States and northwestern Mexico. Researchers discovered that this naturally occurring peptide shared structural similarities with human GLP-1 and possessed potent glucose-lowering properties. While exenatide was inspired by this natural peptide, modern exenatide medications are synthetically produced, not harvested from animals.
However, tirzepatide has no connection to snake venom, Gila monster venom, or any animal-derived compounds. While exenatide's amino acid sequence was based on the naturally occurring exendin-4, tirzepatide represents an entirely different approach. Pharmaceutical scientists at Eli Lilly designed tirzepatide as a synthetic molecule from the ground up, engineering a single peptide chain that could activate both GIP and GLP-1 receptors with optimized potency and duration of action.
This distinction is clinically important for patient counseling. Patients concerned about animal-derived products can be reassured that tirzepatide contains no venom components and is produced through standard pharmaceutical manufacturing processes.
Tirzepatide received FDA approval for type 2 diabetes in May 2022 and for chronic weight management in November 2023, following extensive clinical evaluation through the SURPASS and SURMOUNT trial programs. These rigorous phase 3 studies enrolled over 10,000 participants and demonstrated both efficacy and an acceptable safety profile consistent with the incretin-based medication class.
The most common adverse effects are gastrointestinal in nature, occurring in 20% to 40% of patients. These include nausea, diarrhea, vomiting, constipation, abdominal pain, and dyspepsia. Symptoms are typically mild to moderate in severity, most pronounced during dose escalation, and tend to diminish over time. Gradual dose titration at four-week intervals helps minimize gastrointestinal intolerance. Patients should be counseled to eat smaller meals, avoid high-fat foods, and stay well-hydrated during the initial treatment period.
Serious adverse effects require clinical vigilance. Tirzepatide carries a boxed warning regarding thyroid C-cell tumors, based on rodent studies showing increased incidence of medullary thyroid carcinoma. The medication is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. Other significant risks include acute pancreatitis, hypoglycemia when combined with insulin or sulfonylureas, acute kidney injury (particularly in the setting of severe gastrointestinal symptoms), diabetic retinopathy complications, and gallbladder disease. Zepbound specifically carries a warning about suicidal behavior and ideation, requiring monitoring in patients with a history of depression or suicidal thoughts.
Tirzepatide may reduce the effectiveness of oral contraceptives, particularly during dose initiation and escalation. Patients should use additional or alternative contraception methods for 4 weeks after starting treatment and after each dose increase. The medication is not recommended during pregnancy or breastfeeding, and weight loss is not indicated during pregnancy. It is also not recommended for patients with severe gastrointestinal disease, such as severe gastroparesis.
Patients should be instructed to seek immediate medical attention for severe abdominal pain (potentially indicating pancreatitis), signs of thyroid masses (neck lump, hoarseness, dysphagia), symptoms of hypoglycemia, or severe dehydration. If pancreatitis is suspected, tirzepatide should be promptly discontinued and not restarted if pancreatitis is confirmed. Healthcare providers should monitor renal function in patients with renal impairment and during episodes of severe gastrointestinal adverse reactions. The FDA label provides comprehensive prescribing information that should guide clinical decision-making and patient selection.
Patients frequently express concerns about medication ingredients, particularly with newer therapeutic agents. Tirzepatide contains the active pharmaceutical ingredient (tirzepatide peptide) plus inactive excipients necessary for formulation stability and delivery. According to the FDA label, the inactive ingredients include sodium chloride, sodium phosphate dibasic heptahydrate, sodium hydroxide and/or hydrochloric acid (for pH adjustment), and water for injection. The formulation contains no preservatives and no venom-related substances.
Tirzepatide is a synthetic peptide manufactured in a controlled industrial setting. The final product undergoes extensive purification and quality control testing before distribution. The medication is not derived from animal sources, which may be relevant for patients with specific concerns about medication origins.
Patients with specific dietary restrictions or religious considerations often inquire about animal products. While tirzepatide does not contain direct animal-derived ingredients, patients following vegetarian, vegan, halal, or kosher dietary practices should consult with the manufacturer for specific certification and with religious authorities for guidance on personal circumstances, as manufacturing processes and supply chain components may affect status.
Allergy concerns occasionally arise, particularly regarding peptide medications. The FDA label notes that immunogenicity (antibody formation) has been observed with tirzepatide. True allergic reactions to tirzepatide are rare but possible. Patients should be counseled to recognize signs of hypersensitivity, including rash, itching, difficulty breathing, or swelling of the face, lips, or throat. Anaphylaxis, while extremely uncommon, requires immediate emergency medical attention. Prior allergic reactions to other GLP-1 receptor agonists should be disclosed to healthcare providers, as cross-reactivity is theoretically possible though not well-documented.
For patients with concerns about medication origins or ingredients, healthcare providers should offer clear, evidence-based information and address misconceptions directly. The confusion between tirzepatide and venom-derived medications like exenatide is understandable but scientifically unfounded. Transparent communication about pharmaceutical development and manufacturing processes helps build patient confidence and medication adherence.
No, tirzepatide is entirely synthetic and contains no animal-derived ingredients or venom components. The medication is manufactured through standard pharmaceutical processes using the active ingredient tirzepatide peptide plus inactive excipients including sodium chloride, sodium phosphate, and water for injection.
The confusion arises from exenatide (Byetta), an earlier diabetes medication inspired by exendin-4, a peptide found in Gila monster saliva. However, tirzepatide was designed from the ground up as a synthetic dual GIP/GLP-1 receptor agonist with no connection to reptile biology or venom.
The most common adverse effects are gastrointestinal, occurring in 20-40% of patients, including nausea, diarrhea, vomiting, constipation, and abdominal pain. These symptoms are typically mild to moderate, most pronounced during dose escalation, and tend to diminish over time with gradual titration.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.