LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Not pooping on tirzepatide is a common concern for patients using this dual GIP/GLP-1 receptor agonist medication. Approved by the FDA as Mounjaro for type 2 diabetes and Zepbound for chronic weight management, tirzepatide slows gastrointestinal motility as part of its therapeutic mechanism. This delayed transit can lead to constipation in 12-26% of patients, depending on dose and indication. While uncomfortable, medication-induced constipation is typically manageable through dietary modifications, increased hydration, fiber supplementation, and over-the-counter remedies. Understanding why this occurs and implementing proactive strategies helps patients maintain bowel regularity while benefiting from tirzepatide's glycemic and weight management effects.
Quick Answer: Tirzepatide causes constipation in 12-26% of patients by slowing gastrointestinal motility through GLP-1 receptor activation, which delays transit time and increases water reabsorption from the colon.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). While highly effective for glycemic control and weight loss, tirzepatide's mechanism of action can affect gastrointestinal motility, potentially leading to constipation in some patients.
The drug works primarily through GLP-1 receptor activation throughout the gastrointestinal tract, which slows gastric emptying and reduces intestinal motility. This delayed transit time contributes to better glucose regulation and promotes satiety—key factors in its therapeutic benefits. However, when food and waste material move more slowly through the digestive system, water is reabsorbed more extensively from the colon, potentially resulting in harder, drier stools that are difficult to pass.
Importantly, the gastric emptying delay tends to attenuate with continued therapy (tachyphylaxis), which may explain why some gastrointestinal effects improve over time. Additionally, tirzepatide may reduce appetite, which could lead to decreased food and fluid intake in some patients, potentially contributing to constipation risk.
Constipation associated with tirzepatide is considered a recognized effect related to its GLP-1 activity. Understanding this pharmacological basis helps patients and clinicians anticipate and proactively manage this adverse effect. It is important to note that while uncomfortable, medication-induced constipation is generally manageable with appropriate interventions and does not typically require discontinuation of therapy in most cases.
Of note, tirzepatide is not recommended for patients with severe gastrointestinal disease, including severe gastroparesis.
According to the FDA prescribing information for tirzepatide, constipation is reported as a common gastrointestinal adverse effect, though it occurs less frequently than nausea, diarrhea, and vomiting. In the SURPASS clinical trial program for type 2 diabetes (Mounjaro), constipation was reported in approximately 12-17% of patients across the 5 mg, 10 mg, and 15 mg weekly doses, with higher rates generally observed at higher doses.
In the SURMOUNT trials evaluating tirzepatide for chronic weight management (Zepbound), constipation occurred in 17-26% of patients depending on the dose, compared to 4% in the placebo group. As with other gastrointestinal effects, constipation was more common during the dose escalation period and tended to decrease over time for many patients.
Importantly, constipation severity varies considerably among individuals. Most cases are mild to moderate and occur during the initial titration phase or following dose escalation. Many patients experience transient changes in bowel frequency that improve within several weeks as the body adapts to the medication. However, some patients develop persistent constipation requiring ongoing management strategies.
Gastrointestinal side effects, including constipation, are a primary reason some patients may need to delay dose escalation or temporarily reduce their dose. The FDA-approved prescribing information notes that clinicians may consider delaying dose increases or temporarily decreasing the dose if patients experience troublesome gastrointestinal side effects. This individualized approach to dosing (with maintenance doses of 5 mg, 10 mg, or 15 mg based on response and tolerability) can help optimize both efficacy and tolerability.
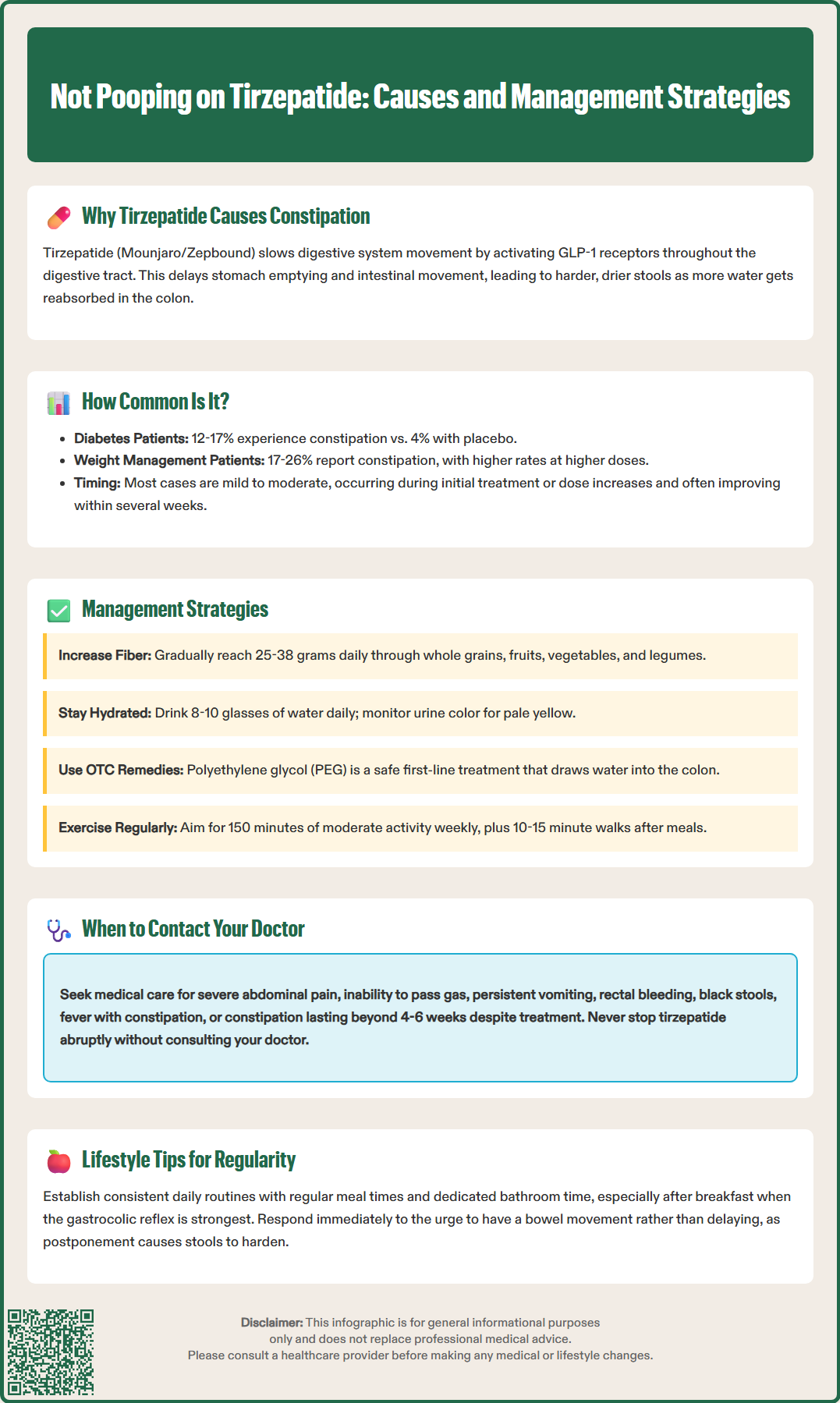
Effective management of tirzepatide-induced constipation typically involves a stepwise approach, beginning with conservative measures and progressing to pharmacological interventions when necessary. According to the 2023 American Gastroenterological Association (AGA) guidelines, soluble fiber supplements and osmotic laxatives like polyethylene glycol (PEG) are recommended as first-line treatments for chronic constipation.
First-line interventions include increasing dietary fiber intake to 25-30 grams daily for women and 30-38 grams daily for men through whole grains, fruits, vegetables, and legumes. Soluble fiber supplements (psyllium, methylcellulose) are particularly effective for softening stools. However, fiber should be increased gradually to avoid bloating and gas, and must be accompanied by adequate fluid intake. Patients should be counseled that fiber without sufficient hydration can paradoxically worsen constipation.
Over-the-counter options provide additional relief when dietary measures prove insufficient:
Osmotic laxatives (polyethylene glycol 3350) draw water into the colon and are generally safe for regular use
Stool softeners (docusate sodium) may help but have limited evidence for chronic constipation
Stimulant laxatives (bisacodyl, senna) are effective for short-term or rescue use but not recommended for long-term management
Magnesium-based products (magnesium hydroxide/citrate) should be used cautiously, especially in patients with kidney disease
Regular physical activity—at least 150 minutes of moderate exercise weekly—promotes intestinal motility. Even brief walks after meals can stimulate bowel function. Establishing a consistent bathroom routine, particularly after breakfast when the gastrocolic reflex is strongest, helps maintain regularity.
If constipation persists despite these measures, healthcare providers may consider temporarily delaying dose increases or reducing the tirzepatide dose. For persistent symptoms, prescription medications such as lubiprostone, linaclotide, plecanatide, or prucalopride may be appropriate for some patients after medical evaluation.
While mild constipation on tirzepatide is common and manageable, certain symptoms warrant prompt medical evaluation. Patients should contact their healthcare provider if they experience several days without a bowel movement despite using over-the-counter remedies, especially if accompanied by significant discomfort, as this may indicate more significant intestinal dysmotility requiring medical intervention.
Red flag symptoms requiring urgent assessment include:
Severe abdominal pain or distension that is progressive or unrelieved
Nausea and vomiting, particularly if unable to tolerate oral intake
Inability to pass gas or persistent vomiting (possible signs of obstruction)
Rectal bleeding or black, tarry stools suggesting gastrointestinal bleeding
Unintentional weight loss beyond expected therapeutic effects
Fever accompanying constipation, which may indicate infection or inflammation
Signs of dehydration (extreme thirst, dry mouth, dizziness, dark urine)
Patients with pre-existing gastrointestinal conditions—including inflammatory bowel disease, previous bowel obstruction, or diverticular disease—should have lower thresholds for seeking medical advice. These individuals may be at higher risk for complications from medication-induced constipation and may require specialized management strategies.
Persistent constipation lasting beyond 4-6 weeks despite appropriate conservative management should prompt re-evaluation. The healthcare provider may need to assess for alternative causes including hypothyroidism, electrolyte abnormalities, or other medications contributing to reduced bowel motility. In some cases, dose adjustment of tirzepatide may be necessary, though this should be balanced against glycemic control and weight management goals.
It is important to note that tirzepatide is not recommended for patients with severe gastroparesis. Symptoms of gastroparesis include persistent nausea, vomiting undigested food, early satiety, and abdominal pain. Patients should never abruptly stop tirzepatide without consulting their prescribing physician, as this decision requires careful consideration of the risk-benefit profile.
Implementing evidence-based dietary and lifestyle modifications can significantly reduce constipation risk and improve quality of life for patients taking tirzepatide. These strategies work synergistically with the medication's therapeutic effects while minimizing gastrointestinal adverse effects.
Hydration optimization is foundational. Most adults should aim for adequate daily fluid intake (approximately 8-10 glasses of water daily), with needs varying based on activity level, climate, and individual health status. Patients with heart failure or kidney disease should follow their healthcare provider's specific fluid recommendations. Starting each day with warm water or herbal tea may stimulate bowel activity. While maintaining adequate overall hydration, patients can monitor hydration through urine color, aiming for pale yellow rather than dark or concentrated urine.
Strategic fiber intake requires both quantity and quality considerations. The Dietary Guidelines for Americans recommend 25-30 grams of fiber daily for women and 30-38 grams for men, with attention to fiber type:
Soluble fiber (oats, psyllium, apples, beans) forms a gel that softens stools
Insoluble fiber (wheat bran, vegetables, whole grains) adds bulk and promotes transit
Patients should increase fiber gradually over 2-3 weeks to minimize bloating. Fiber supplements like psyllium husk (Metamucil) or methylcellulose (Citrucel) can bridge gaps when dietary intake is insufficient.
Some patients may find that probiotic-rich foods—including yogurt, kefir, sauerkraut, and kimchi—help support regular bowel function, though evidence specific to tirzepatide users is limited.
Physical activity directly stimulates intestinal peristalsis. The U.S. Physical Activity Guidelines recommend 150 minutes of moderate-intensity aerobic activity weekly, but even 10-15 minute walks after meals can promote bowel movements. Some patients find that gentle yoga or stretching that involves abdominal movement may provide additional benefit, though evidence is limited.
Establishing a consistent daily routine—including regular meal times and dedicated bathroom time—helps regulate the body's natural circadian rhythm of bowel function. Patients should respond promptly to defecation urges rather than delaying, as postponement can lead to progressive stool hardening and more difficult evacuation.
Moderate coffee consumption may stimulate bowel movements in some individuals, though overall hydration remains the priority.
Constipation on tirzepatide is most common during the initial titration phase and following dose escalations, with many patients experiencing improvement within several weeks as the body adapts. Some patients may develop persistent constipation requiring ongoing management strategies throughout treatment.
According to American Gastroenterological Association guidelines, osmotic laxatives like polyethylene glycol (PEG 3350) are recommended as first-line treatment for tirzepatide-induced constipation, as they are generally safe for regular use and effectively draw water into the colon to soften stools.
Patients should not abruptly stop tirzepatide without consulting their prescribing physician. Most constipation cases are manageable with dietary modifications, hydration, fiber supplementation, and over-the-counter remedies, though dose adjustment may be considered if symptoms persist despite appropriate management.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.