LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Do you have to taper off tirzepatide when stopping treatment? Unlike medications that cause withdrawal symptoms, tirzepatide (Mounjaro, Zepbound) does not require gradual dose reduction from a pharmacological standpoint. The FDA prescribing information does not mandate tapering when discontinuing this dual GIP/GLP-1 receptor agonist. However, the clinical approach to stopping tirzepatide depends on your underlying condition—whether type 2 diabetes or chronic weight management—and requires careful medical planning. Understanding the difference between pharmacological necessity and clinical strategy helps patients and providers make informed decisions about safely discontinuing tirzepatide while maintaining optimal health outcomes.
Quick Answer: Tirzepatide does not require tapering from a pharmacological perspective, as the FDA prescribing information does not mandate gradual dose reduction when stopping treatment.
Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management and chronic weight management. As a once-weekly subcutaneous injection, tirzepatide works by enhancing insulin secretion in response to meals, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways.
Many patients and clinicians wonder about the proper approach to discontinuing tirzepatide, particularly whether a gradual dose reduction is medically necessary. Unlike certain medications such as corticosteroids, beta-blockers, or benzodiazepines—where abrupt cessation can trigger withdrawal syndromes or rebound effects—tirzepatide does not cause physiological dependence or withdrawal symptoms. The FDA prescribing information for tirzepatide does not require tapering when discontinuing treatment.
The decision to stop tirzepatide may arise from various circumstances: achievement of treatment goals, intolerable side effects, insurance coverage changes, cost considerations, pregnancy, or medical contraindications (including medullary thyroid carcinoma, multiple endocrine neoplasia syndrome type 2, or serious hypersensitivity reactions, as noted in the boxed warning). Each situation requires individualized assessment. While the medication itself does not require tapering from a pharmacological standpoint, the clinical context surrounding discontinuation—particularly the management of underlying conditions like diabetes or obesity—demands careful planning and medical supervision to ensure patient safety and optimize long-term health outcomes.
From a strict pharmacological perspective, tirzepatide does not require tapering before discontinuation. The FDA prescribing information does not mandate a gradual dose reduction protocol when stopping treatment. This differs fundamentally from medications that cause physiological adaptation requiring gradual withdrawal.
Tirzepatide has a half-life of approximately 5 days, meaning the medication naturally clears from your system over several weeks following the last injection. This gradual pharmacokinetic elimination provides a built-in "taper" effect as drug levels progressively decline. While there is no withdrawal syndrome associated with tirzepatide discontinuation, patients should expect changes in blood glucose levels and weight as the medication's effects diminish.
However, the clinical decision about how to stop tirzepatide extends beyond simple pharmacology. The underlying condition being treated—not the medication itself—determines the approach to discontinuation. For patients with type 2 diabetes, stopping tirzepatide means losing its glucose-lowering effects, which may necessitate alternative diabetes management strategies. For those using tirzepatide for weight management, discontinuation typically results in weight regain over time.
Some healthcare providers may choose to implement a stepwise dose reduction (for example, decreasing from 15 mg to 10 mg to 5 mg over several weeks) not because tapering is pharmacologically required, but to allow time for:
Transitioning to alternative therapies
Implementing lifestyle modifications
Monitoring metabolic parameters
Adjusting other medications
Psychological preparation for treatment changes
This approach represents clinical judgment rather than medical necessity. The decision should be individualized based on your specific health status, treatment goals, and the reason for discontinuation.
After stopping tirzepatide, increased blood glucose monitoring is recommended for at least 2-4 weeks. Contact your healthcare provider if you experience persistent fasting glucose above 180 mg/dL, random glucose above 250 mg/dL, or symptoms of hyperglycemia (excessive thirst, frequent urination, blurred vision).
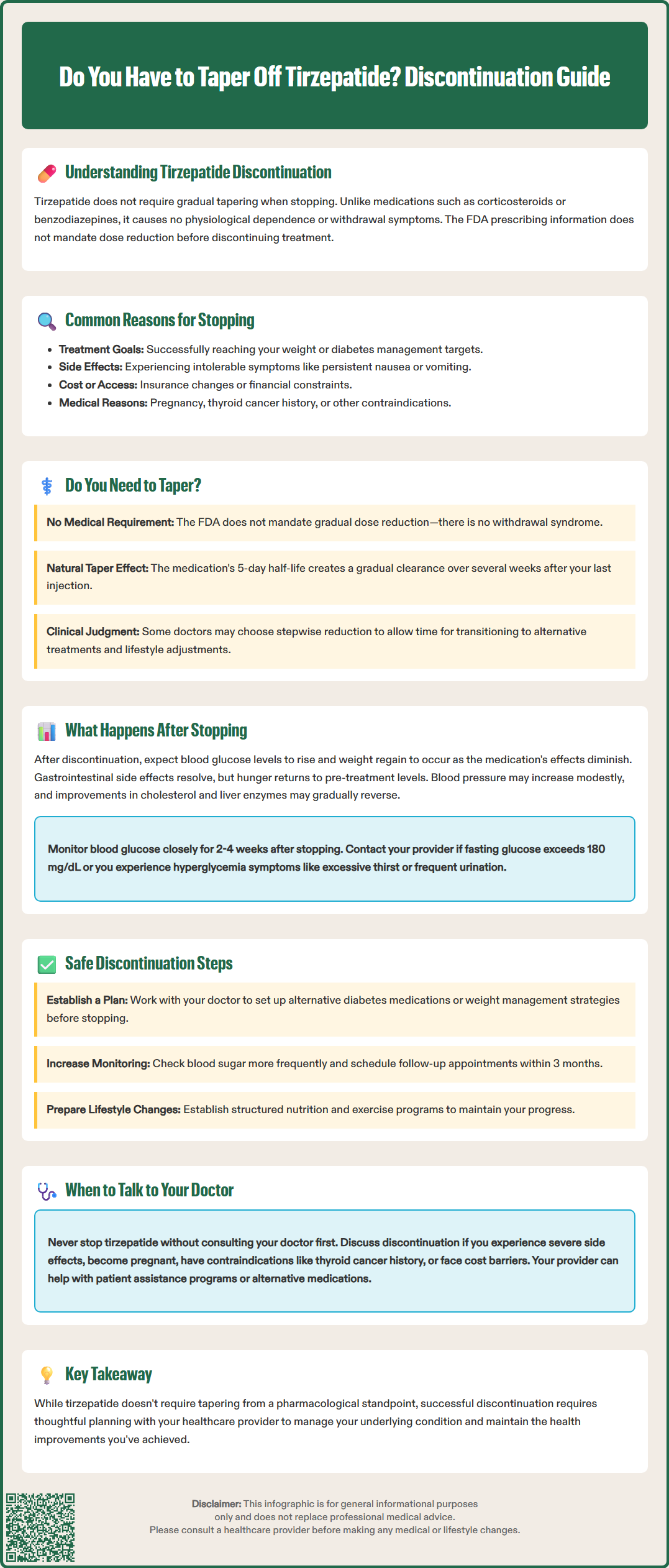
When tirzepatide is discontinued, patients can expect several physiological changes as the medication's effects gradually diminish. Understanding these changes helps set realistic expectations and facilitates appropriate planning.
Metabolic effects: For patients with type 2 diabetes, blood glucose levels typically begin rising as the medication's insulinotropic and glucagon-suppressing effects wane. Glycemic control generally deteriorates progressively after tirzepatide cessation, with HbA1c levels moving toward pre-treatment values without alternative therapy. The rate and magnitude of glucose elevation depend on baseline diabetes severity, duration of disease, beta-cell function, and concurrent medications. Patients should monitor glucose levels closely during this transition period.
Weight changes: Weight regain represents one of the most consistent findings after stopping tirzepatide. Clinical evidence from the SURMOUNT-4 randomized withdrawal study indicates that patients typically regain a substantial portion of lost weight after discontinuation. This occurs because tirzepatide's appetite-suppressing effects—mediated through hypothalamic pathways and delayed gastric emptying—resolve as drug levels decline. Hunger and appetite typically return to pre-treatment levels, and metabolic rate may decrease slightly as body weight had previously declined.
Gastrointestinal symptoms: The gastrointestinal side effects commonly experienced during tirzepatide treatment (nausea, reduced appetite, early satiety) typically resolve after stopping. Some patients report increased appetite and faster return of normal hunger cues, which can feel pronounced after months of appetite suppression.
Cardiovascular and other effects: Blood pressure may increase modestly as weight is regained. Improvements in lipid profiles, liver enzymes, and inflammatory markers observed during treatment may also gradually reverse. As the medication's effects diminish, the underlying disease processes resume their natural course without pharmacological intervention, highlighting the importance of establishing alternative management strategies.
While tirzepatide can be stopped abruptly without medical risk from the medication itself, a thoughtful discontinuation strategy optimizes safety and long-term outcomes. The key principle is managing the underlying condition, not tapering the drug.
For type 2 diabetes management: Before stopping tirzepatide, work with your healthcare provider to establish an alternative diabetes management plan. This may include:
Initiating or optimizing other glucose-lowering medications (metformin, SGLT2 inhibitors, sulfonylureas, or other GLP-1 receptor agonists)
Increasing frequency of blood glucose monitoring to detect hyperglycemia early
Reviewing and intensifying lifestyle modifications (dietary changes, physical activity)
Scheduling follow-up appointments to assess HbA1c within 3 months
Adjusting insulin doses if applicable, as insulin requirements typically increase after stopping tirzepatide
Patients should monitor for signs of significant hyperglycemia (fasting glucose >180 mg/dL, random glucose >250 mg/dL) and contact their provider promptly if these occur. Those with insulin-dependent or advanced diabetes may need more frequent monitoring and medication adjustments to prevent metabolic decompensation. According to ADA Standards of Care, maintaining glycemic targets is essential to prevent long-term complications including retinopathy, nephropathy, neuropathy, and cardiovascular disease.
For weight management: If discontinuing tirzepatide prescribed for obesity, consider:
Establishing a structured nutrition and exercise program before stopping
Transitioning to alternative weight management medications if appropriate
Setting realistic expectations about weight regain
Implementing behavioral strategies and support systems
Regular weight monitoring and early intervention if significant regain occurs
Practical discontinuation steps:
If cost or access issues are driving discontinuation, discuss these openly with your healthcare team, as patient assistance programs, alternative formulations, or therapeutic substitutes may be available.
Never discontinue tirzepatide without consulting your healthcare provider. While the medication itself can be stopped safely, the clinical implications of discontinuation require medical assessment and planning. Several situations warrant immediate discussion with your doctor about potentially stopping or modifying tirzepatide therapy.
Intolerable side effects: If you experience persistent severe nausea, vomiting, diarrhea, or abdominal pain that significantly impairs quality of life despite dose adjustments and supportive measures, discuss discontinuation. Serious adverse effects requiring immediate medical attention include signs of pancreatitis (severe persistent abdominal pain radiating to the back), symptoms suggesting thyroid tumors (neck mass, difficulty swallowing, persistent hoarseness), severe allergic reactions, or acute kidney injury (significantly decreased urination, swelling, fatigue).
Pregnancy: According to FDA labeling, tirzepatide should be discontinued when pregnancy is recognized. If you are planning pregnancy, consult your healthcare provider about the appropriate timing for discontinuation and establishing alternative diabetes or weight management strategies safe for pregnancy.
Medical contraindications: Tirzepatide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC), in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2), and in those with serious hypersensitivity to tirzepatide. Additionally, tirzepatide is not recommended for patients with severe gastrointestinal disease, including severe gastroparesis. While no dose adjustment is required for renal impairment, patients with kidney issues should be monitored for potential dehydration and kidney injury, especially if experiencing severe gastrointestinal adverse reactions.
Financial or access barriers: If cost or insurance coverage changes make tirzepatide unaffordable, discuss this proactively with your provider rather than simply stopping. Alternative medications, patient assistance programs, or modified treatment plans may be available.
Achievement of treatment goals: Some patients reach their diabetes or weight management targets and wonder if continued treatment is necessary. This decision requires careful discussion about maintenance therapy, risk of relapse, and long-term management strategies. For most patients with type 2 diabetes or obesity, these represent chronic conditions requiring ongoing management rather than short-term treatment.
Your healthcare provider can help assess whether discontinuation is appropriate, establish monitoring protocols, arrange alternative therapies if needed, and ensure safe transition off tirzepatide while maintaining optimal management of your underlying health conditions.
Yes, tirzepatide can be stopped abruptly without causing withdrawal symptoms or physiological dependence. However, you should always consult your healthcare provider before discontinuing to establish appropriate monitoring and alternative management strategies for your underlying diabetes or weight condition.
Blood glucose levels typically begin rising after stopping tirzepatide as the medication's insulin-enhancing and glucagon-suppressing effects diminish. Without alternative diabetes management, HbA1c levels generally move toward pre-treatment values, requiring increased monitoring and potential medication adjustments.
Weight regain is common after discontinuing tirzepatide, as the medication's appetite-suppressing effects and delayed gastric emptying resolve. Clinical studies show patients typically regain a substantial portion of lost weight without continued treatment or alternative weight management strategies.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.