LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide, marketed as Mounjaro for type 2 diabetes and Zepbound for weight management, is a dual GIP/GLP-1 receptor agonist that has generated interest regarding its potential effects on erectile dysfunction. While tirzepatide is not FDA-approved for treating erectile dysfunction and lacks direct mechanisms targeting sexual function, its significant impact on diabetes control and weight reduction may indirectly influence erectile health. Men with diabetes experience erectile dysfunction at rates of 50-75%, driven by vascular damage, neuropathy, and hormonal changes that tirzepatide's metabolic benefits might address. Understanding the relationship between tirzepatide and erectile dysfunction requires examining both the medication's established effects and the complex connections between metabolic health and sexual function.
Quick Answer: Tirzepatide is not FDA-approved for erectile dysfunction and has no direct mechanism targeting sexual function, though its effects on diabetes control and weight loss may indirectly improve erectile health over time.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (Mounjaro) and chronic weight management (Zepbound). For weight management, it is indicated for adults with a BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related comorbidity.
The medication works through a dual mechanism of action. By activating both GIP and GLP-1 receptors, tirzepatide enhances insulin secretion in a glucose-dependent manner, suppresses glucagon release, slows gastric emptying, and reduces appetite. This combined effect leads to improved glycemic control and substantial weight reduction. Clinical trials have demonstrated that tirzepatide can reduce hemoglobin A1c by up to 2.5% in type 2 diabetes, with weight loss typically ranging from 5-10% in diabetes patients and 15-20% in those treated specifically for obesity.
Tirzepatide is administered as a once-weekly subcutaneous injection, starting at 2.5 mg for 4 weeks and then increasing in 2.5 mg increments to a maintenance dose of 5-15 mg based on clinical response and tolerability. Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhea, and constipation, which typically diminish over time. More serious risks include hypoglycemia (particularly when used with insulin or sulfonylureas), acute kidney injury, pancreatitis, gallbladder disease, and potential thyroid C-cell tumors (based on animal studies). The medication is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2, and is not indicated for type 1 diabetes or use with other GLP-1 receptor agonists.
Patients using oral contraceptives should use additional contraception for 4 weeks after initiating tirzepatide or after dose increases due to potential reduced effectiveness. Tirzepatide should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
While tirzepatide's primary indications focus on metabolic health, its effects on weight loss and glycemic control may have secondary benefits for various obesity- and diabetes-related complications, though cardiovascular outcome trials are still ongoing.
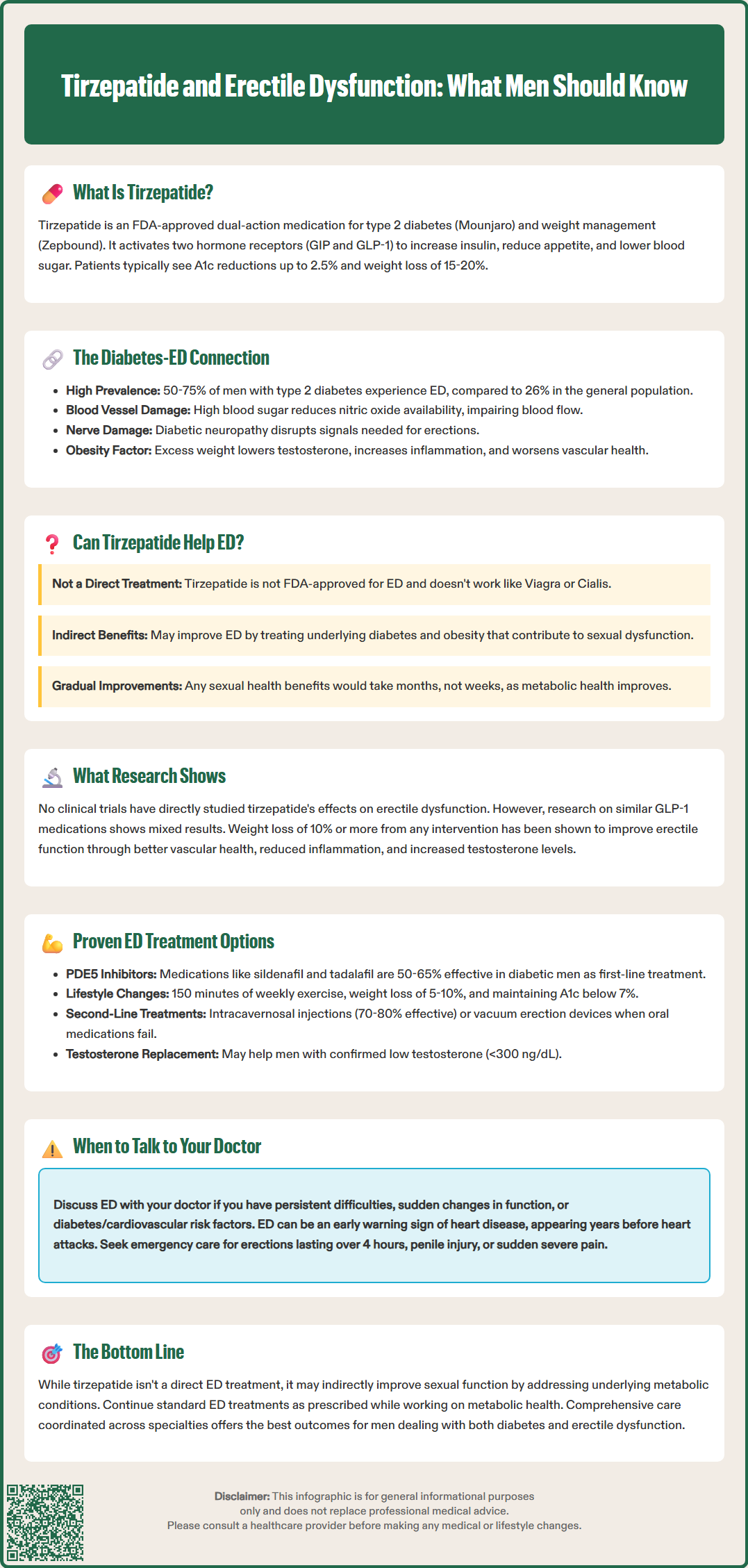
Erectile dysfunction (ED) is a highly prevalent complication in men with type 2 diabetes, affecting approximately 50-75% of diabetic men compared to about 26% in the general male population, with rates varying by age and diabetes duration. The relationship between diabetes and erectile function is multifactorial, involving vascular, neurological, hormonal, and psychological mechanisms that collectively impair the ability to achieve or maintain an erection sufficient for sexual activity.
Diabetes contributes to ED primarily through endothelial dysfunction and vascular damage. Chronic hyperglycemia leads to advanced glycation end products, oxidative stress, and inflammation that damage the blood vessels supplying the penis. This vascular impairment reduces nitric oxide availability, a critical molecule for smooth muscle relaxation and arterial dilation necessary for erection. Additionally, diabetic neuropathy can damage the autonomic nerves controlling erectile function, further compromising sexual response. Men with poorly controlled diabetes typically experience more severe ED at younger ages compared to those with well-managed blood glucose levels.
Obesity independently contributes to erectile dysfunction through multiple pathways. Excess adipose tissue, particularly visceral fat, promotes systemic inflammation and insulin resistance while reducing testosterone levels through increased aromatase activity that converts testosterone to estrogen. Lower testosterone is associated with reduced libido and erectile quality. Obesity also increases the risk of hypertension and dyslipidemia, both of which damage vascular health and contribute to ED.
Certain medications commonly prescribed for diabetes-related conditions, including some antihypertensives (particularly thiazide diuretics and beta-blockers) and antidepressants (especially SSRIs), can further contribute to erectile difficulties.
The American Diabetes Association recognizes ED as a diabetes-related complication and recommends routine screening. Weight loss of even 5-10% has been shown to improve erectile function in obese men, while improved glycemic control can slow the progression of both vascular and neurological damage. These observations suggest that interventions addressing both diabetes and obesity may offer benefits for sexual health, though the relationship is complex and multifactorial.
There is currently no official FDA indication or established clinical evidence that tirzepatide directly treats erectile dysfunction. Using tirzepatide specifically for ED would be considered off-label and is not supported by clinical trial data. However, the medication's effects on the underlying metabolic conditions that contribute to ED—namely diabetes and obesity—suggest potential indirect benefits for sexual function. It is important to distinguish between direct pharmacological effects on erectile tissue and secondary improvements resulting from better metabolic health.
Tirzepatide does not have a known direct mechanism of action on the vascular or neurological pathways specifically involved in erectile function. Unlike phosphodiesterase-5 (PDE5) inhibitors such as sildenafil or tadalafil, which directly enhance nitric oxide signaling in penile tissue, tirzepatide's primary targets are metabolic receptors in the pancreas, gastrointestinal tract, and brain. The medication does not directly affect smooth muscle relaxation, arterial blood flow to the penis, or nerve conduction in the manner required for immediate erectile improvement.
Nevertheless, by addressing the root causes of metabolic dysfunction, tirzepatide may create conditions more favorable for erectile function over time. Significant weight loss can reduce systemic inflammation, improve testosterone levels, and enhance vascular health throughout the body, including the penile vasculature. Improved glycemic control may slow or partially reverse diabetic vascular and nerve damage, potentially preserving or improving erectile capacity. Additionally, weight loss often improves self-esteem, body image, and psychological well-being, which can positively influence sexual confidence and performance.
Patients should understand that any potential benefits for erectile function would likely be gradual and secondary to metabolic improvements rather than immediate or direct. ED has multiple contributing factors, and while optimizing diabetes and weight management is important, it may not fully resolve erectile difficulties, particularly in men with advanced vascular disease or significant neuropathy. Standard ED treatments should be continued as recommended by healthcare providers while addressing metabolic health. A comprehensive approach addressing all contributing factors is typically necessary for optimal outcomes.
Research specifically examining tirzepatide's effects on erectile dysfunction remains limited, with no randomized controlled trials evaluating erectile function as a primary or secondary endpoint. The landmark SURPASS clinical trial program, which established tirzepatide's efficacy for diabetes management, did not include erectile function as an outcome measure. Similarly, the SURMOUNT trials evaluating tirzepatide for weight management did not systematically assess sexual health outcomes, leaving a significant gap in our understanding of this medication's impact on ED.
Broader research on GLP-1 receptor agonists (such as semaglutide and liraglutide) has shown mixed results regarding sexual function. Some observational studies have reported improvements in erectile function scores among men with diabetes who achieved significant weight loss and better glycemic control with GLP-1 therapies. A systematic review found that metabolic improvements associated with GLP-1 agonists correlated with modest improvements in International Index of Erectile Function (IIEF) scores, though the evidence quality was considered low to moderate. These improvements appeared most pronounced in men with obesity and poorly controlled diabetes at baseline.
Weight loss interventions more generally have demonstrated benefits for erectile function. Studies of bariatric surgery and intensive lifestyle modification show that men losing 10% or more of body weight often experience measurable improvements in erectile function, likely mediated through improved endothelial function, reduced inflammation, and increased testosterone levels. Given that tirzepatide produces substantial weight loss, particularly in patients with obesity, similar benefits might theoretically occur, though this remains speculative without dedicated research.
Importantly, the timeline for potential sexual health benefits would likely extend over months rather than weeks, corresponding to the gradual metabolic improvements achieved with tirzepatide therapy. Patients should not expect immediate changes in erectile function upon starting the medication. Ongoing research, including post-marketing surveillance and dedicated sexual health studies, will be necessary to definitively characterize tirzepatide's impact on erectile dysfunction and other aspects of sexual health in men with diabetes and obesity.
Men with diabetes and erectile dysfunction have access to multiple evidence-based treatment options that can be used individually or in combination. The American Urological Association and American College of Physicians recommend a stepwise approach beginning with lifestyle modification and oral medications, progressing to more invasive interventions if necessary.
First-line treatments include:
PDE5 inhibitors (sildenafil, tadalafil, vardenafil, avanafil): These medications enhance nitric oxide signaling and remain the most effective oral treatment for ED, with success rates of 50-65% in diabetic men (somewhat lower than in non-diabetic populations). They are generally safe but contraindicated with nitrate medications and riociguat, and require caution in men with cardiovascular disease or those taking alpha-blockers. Specific nitrate washout periods (24-48 hours depending on the agent) should be observed if switching between these medications.
Lifestyle modifications: Weight loss, regular exercise, smoking cessation, and alcohol moderation can improve erectile function. The ADA recommends at least 150 minutes of moderate-intensity aerobic activity weekly.
Glycemic optimization: Maintaining hemoglobin A1c below 7% (or individualized targets) may slow progression of diabetic complications affecting sexual function.
Psychosexual therapy: Counseling can address psychological factors contributing to ED, particularly helpful as an adjunct to medical therapy.
Second-line treatments for men who do not respond adequately to oral medications include:
Intracavernosal injections (alprostadil, combination therapies): These medications are injected directly into the penis before sexual activity, producing erections in 70-80% of users. Proper training in injection technique is essential.
Intraurethral suppositories (alprostadil): A less invasive alternative to injections, though generally less effective.
Vacuum erection devices: Mechanical devices that draw blood into the penis, secured with a constriction ring. Non-pharmacological and safe for most men.
Third-line treatments include penile prosthesis implantation, reserved for men who have failed or cannot tolerate less invasive options. These surgically implanted devices have high satisfaction rates but are irreversible.
Addressing cardiovascular risk factors is crucial, as ED often serves as an early marker of systemic vascular disease. The Princeton IV Consensus provides guidance for cardiovascular risk stratification in men with ED. Men with new-onset ED should undergo cardiovascular risk assessment, including blood pressure, lipid profile, and consideration of stress testing when appropriate. Testosterone replacement may benefit men with documented hypogonadism (typically defined as morning total testosterone <300 ng/dL confirmed on two separate occasions), though it does not directly improve erectile function in eugonadal men.
A comprehensive approach addressing diabetes management, weight optimization (potentially including medications like tirzepatide), cardiovascular health, and specific ED treatments offers the best outcomes for sexual health in diabetic men.
Sexual health is an important component of overall well-being and quality of life, yet many men hesitate to discuss erectile difficulties with healthcare providers due to embarrassment or misconceptions. The American Diabetes Association and American Urological Association recommend that clinicians routinely screen men with diabetes for sexual dysfunction, and patients should feel empowered to initiate these conversations proactively.
You should discuss erectile concerns with your doctor if:
You experience persistent difficulty achieving or maintaining erections sufficient for sexual activity
Erectile problems cause distress or relationship difficulties
You notice sudden changes in erectile function, which may indicate cardiovascular issues
You have diabetes or other conditions known to affect sexual health
You are starting or changing medications that might impact erectile function
You experience reduced libido, which may indicate hormonal issues requiring evaluation
Seek immediate medical attention for these urgent conditions:
Priapism (erection lasting >4 hours)
Penile injury or trauma
Sudden onset of severe penile pain or curvature
Erectile dysfunction can serve as an early warning sign of cardiovascular disease, often preceding heart attacks or strokes by several years. Men experiencing new or worsening ED should undergo cardiovascular risk assessment, particularly if they have diabetes, hypertension, high cholesterol, or smoking history. The Princeton IV Consensus provides guidance on risk stratification and evaluation. This assessment typically includes blood pressure measurement, lipid panel, hemoglobin A1c, and potentially additional cardiac testing based on risk factors.
When discussing sexual health, be prepared to provide information about the onset and duration of symptoms, the presence of morning or spontaneous erections (which help distinguish vascular from psychological causes), current medications, and any relationship or psychological factors. Your doctor should assess testosterone levels if you have symptoms of hypogonadism, particularly if you also experience fatigue, reduced muscle mass, or mood changes. Morning total testosterone below 300 ng/dL should be confirmed with a second measurement, and additional testing (LH, prolactin) may be warranted if low testosterone is confirmed. A thorough medication review is essential, as numerous drugs—including certain blood pressure medications, antidepressants, and others—can contribute to erectile difficulties.
If you are taking or considering tirzepatide for diabetes or weight management, discuss your sexual health goals with your prescribing physician. While the medication may indirectly benefit erectile function through metabolic improvements, it should be viewed as part of a comprehensive treatment strategy rather than a specific ED therapy. Your doctor can help coordinate care between endocrinology, primary care, urology, and cardiology as needed to address all aspects of your metabolic and sexual health. Remember that effective treatments exist for erectile dysfunction, and addressing the issue openly with your healthcare team is the first step toward improvement.
No, tirzepatide is not FDA-approved for erectile dysfunction and has no direct mechanism targeting sexual function. Any potential benefits would be indirect, resulting from improved diabetes control and weight loss over time rather than immediate effects on erectile tissue.
If sexual health improvements occur, they would likely develop gradually over months as metabolic health improves, not immediately. Benefits would correspond to progressive weight loss, better glycemic control, and reduced inflammation rather than rapid pharmacological effects.
PDE5 inhibitors like sildenafil and tadalafil remain first-line treatment with 50-65% success rates in diabetic men. A comprehensive approach including glycemic optimization, lifestyle modifications, cardiovascular risk management, and specific ED therapies offers the best outcomes.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.