LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide, marketed as Mounjaro for type 2 diabetes and Zepbound for weight management, is a dual GIP/GLP-1 receptor agonist that has transformed metabolic disease treatment. While patients may wonder about tirzepatide and yeast infections, current evidence shows no direct causal link between this medication and fungal infections. Unlike SGLT2 inhibitors that increase infection risk through glucosuria, tirzepatide improves glycemic control without causing glucose spillage into urine. Understanding the relationship between diabetes medications and infection risk helps patients make informed decisions about their treatment while implementing appropriate preventive strategies.
Quick Answer: Tirzepatide does not directly cause yeast infections and is not associated with increased fungal infection rates in clinical trials, unlike SGLT2 inhibitors.
Tirzepatide is a novel dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight loss), tirzepatide works through a dual mechanism of action that enhances insulin secretion, suppresses glucagon release, slows gastric emptying, and reduces appetite. This unique pharmacological profile has demonstrated significant efficacy in improving glycemic control and promoting substantial weight loss in clinical trials.
The most commonly reported adverse effects of tirzepatide are gastrointestinal in nature, occurring in a substantial proportion of patients during initial treatment and dose escalation. These include nausea, diarrhea, vomiting, constipation, abdominal pain, and decreased appetite. According to FDA prescribing information, gastrointestinal side effects are typically mild to moderate in severity and tend to diminish over time as patients develop tolerance to the medication. To minimize these effects, tirzepatide is initiated at a low dose (2.5 mg once weekly) and gradually increased every 4 weeks.
Other notable adverse effects include injection site reactions, fatigue, and potential hypoglycemia when tirzepatide is used in combination with insulin or insulin secretagogues such as sulfonylureas. Rare but serious risks include pancreatitis, gallbladder disease, acute kidney injury, and hypersensitivity reactions. Patients should stop taking tirzepatide and seek immediate medical attention if they experience severe abdominal pain (possibly radiating to the back) with or without vomiting, as this may indicate pancreatitis.
The FDA label carries a boxed warning regarding thyroid C-cell tumors observed in rodent studies, though the relevance to humans remains uncertain. Tirzepatide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2). It is also not recommended for patients with severe gastrointestinal disease, including severe gastroparesis, and is not indicated for use in type 1 diabetes. Healthcare providers must balance the substantial metabolic benefits of tirzepatide against its side effect profile when making treatment decisions for individual patients.
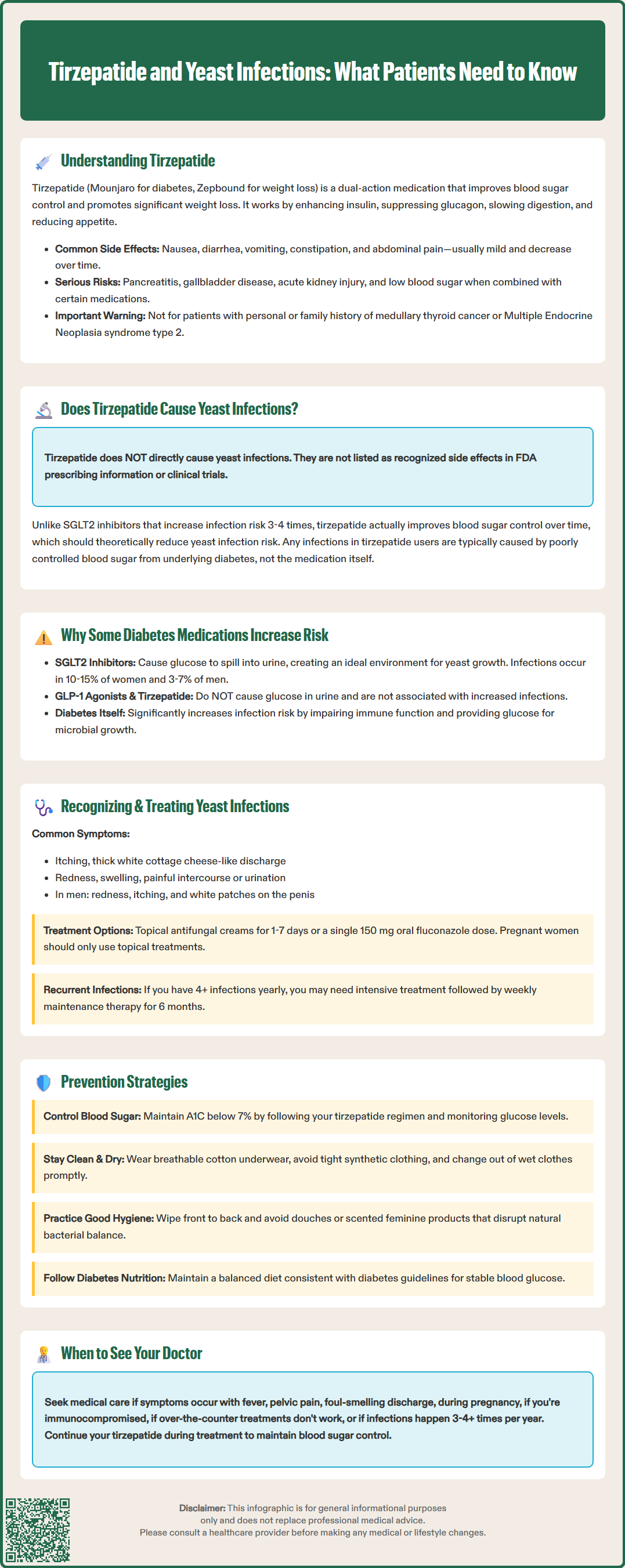
There is no established direct causal relationship between tirzepatide and yeast infections based on current clinical evidence. Yeast infections, particularly vulvovaginal candidiasis in women and less commonly balanitis in men, are not listed as recognized adverse effects in the FDA prescribing information for tirzepatide. Clinical trials evaluating tirzepatide safety, including the SURPASS and SURMOUNT trial programs, did not identify genitourinary fungal infections as a significant concern compared to placebo or active comparators. This distinguishes tirzepatide from sodium-glucose cotransporter-2 (SGLT2) inhibitors, a class of diabetes medications with a well-documented association with increased rates of genital mycotic infections.
However, the relationship between tirzepatide and infection risk is more nuanced than a simple absence of direct causation. Patients taking tirzepatide may experience yeast infections due to underlying factors related to their diabetes rather than the medication itself. Poorly controlled blood glucose creates an environment conducive to Candida overgrowth, as elevated glucose levels in bodily fluids and tissues provide an ideal substrate for fungal proliferation. While tirzepatide improves glycemic control and should theoretically reduce infection risk over time, patients may still have periods of hyperglycemia, particularly during treatment initiation or if adherence is suboptimal.
Additionally, the substantial weight loss associated with tirzepatide therapy may indirectly influence infection risk. Obesity itself is a risk factor for certain types of candidal infections, particularly in skin folds (intertriginous candidiasis), and weight loss may actually reduce this risk by decreasing skin-to-skin contact areas and moisture retention. It is important to emphasize that any yeast infections occurring in patients taking tirzepatide are more likely attributable to diabetes-related factors, individual susceptibility, or concurrent conditions rather than a direct pharmacological effect of the medication itself. Patients concerned about recurrent infections should undergo comprehensive evaluation to identify underlying contributing factors.
The relationship between diabetes medications and infection risk varies considerably depending on the drug class and mechanism of action. SGLT2 inhibitors such as canagliflozin, dapagliflozin, and empagliflozin have a well-established association with increased rates of genitourinary fungal infections. These medications work by blocking glucose reabsorption in the proximal renal tubule, resulting in glucosuria (glucose in the urine). The presence of glucose in the urogenital tract creates an optimal environment for Candida species to proliferate, leading to vulvovaginal candidiasis in women and balanitis or balanoposthitis in men. According to FDA prescribing information, genital mycotic infections occur in approximately 10-15% of women and 3-7% of men taking SGLT2 inhibitors, with rates varying by specific agent, patient sex, and circumcision status in men, representing a three- to fourfold increase compared to placebo.
In contrast, incretin-based therapies, including GLP-1 receptor agonists (like semaglutide and dulaglutide) and the dual GIP/GLP-1 receptor agonist tirzepatide, do not cause glucosuria and therefore lack this specific mechanism for promoting fungal infections. These medications enhance glucose-dependent insulin secretion and suppress glucagon, thereby lowering blood glucose through physiological pathways rather than urinary glucose excretion. The absence of glucosuria explains why these agents are not associated with increased rates of genitourinary infections in clinical trials.
However, diabetes itself remains a significant risk factor for various infections, including yeast infections, regardless of medication use. Chronic hyperglycemia impairs multiple aspects of immune function, including neutrophil chemotaxis, phagocytosis, and cell-mediated immunity. Elevated glucose levels in tissues and secretions provide substrate for microbial growth. Diabetic patients also experience microvascular complications affecting skin integrity and healing capacity. The American Diabetes Association emphasizes that optimal glycemic control is fundamental to reducing infection risk in people with diabetes. Therefore, medications that improve glucose control, including tirzepatide, should theoretically reduce long-term infection susceptibility by addressing the underlying metabolic dysfunction, even though they do not directly cause infections through their mechanism of action.
Recognizing yeast infections promptly is essential for effective management and preventing complications. Vulvovaginal candidiasis typically presents with vulvar pruritus (itching), vaginal discharge that is characteristically thick, white, and cottage cheese-like in appearance, vulvar erythema and edema, and dyspareunia (painful intercourse). Some women also experience dysuria (painful urination) or vulvar burning. Male genital candidiasis manifests as erythema, pruritus, and sometimes white plaques on the glans penis or under the foreskin, often accompanied by discomfort or pain. Cutaneous candidiasis in skin folds may present with erythematous, macerated patches with satellite lesions.
Patients should seek medical evaluation if they experience these symptoms, particularly if accompanied by fever, pelvic or abdominal pain, malodorous discharge, if they are pregnant or immunocompromised, if symptoms are severe, if over-the-counter treatments fail, or if infections recur (≥3-4 episodes per year).
Diagnosis is typically clinical, based on characteristic symptoms and physical examination findings. Microscopic examination of vaginal discharge prepared with potassium hydroxide (KOH) can reveal budding yeast and pseudohyphae, confirming the diagnosis. Vaginal pH testing shows a normal pH (less than 4.5) in candidiasis, helping distinguish it from bacterial vaginosis or trichomoniasis. Culture or PCR testing may be indicated for recurrent infections or when non-albicans Candida species are suspected, as these may require alternative antifungal therapy.
According to CDC Sexually Transmitted Infections Treatment Guidelines, treatment for uncomplicated vulvovaginal candidiasis includes topical azole antifungals such as clotrimazole, miconazole, or terconazole applied intravaginally for 1-7 days, or oral fluconazole 150 mg as a single dose. Topical and oral therapies have comparable efficacy for uncomplicated infections. For pregnant women, only topical azole therapies for 7 days are recommended; oral fluconazole should be avoided during pregnancy. For male genital candidiasis, topical azole creams applied twice daily for 7-14 days are typically effective.
Patients with recurrent vulvovaginal candidiasis (four or more episodes annually) require more intensive treatment: an induction phase with fluconazole 150 mg every 72 hours for 2-3 doses or 10-14 days of topical therapy, followed by maintenance therapy with fluconazole 100-200 mg weekly for 6 months. Patients taking tirzepatide should continue their diabetes medication as prescribed during treatment for yeast infections, as discontinuation could worsen glycemic control and potentially exacerbate infection susceptibility. Any concerns about medication interactions should be discussed with a healthcare provider or pharmacist.
Preventing yeast infections in patients taking tirzepatide centers primarily on optimizing diabetes management and implementing practical hygiene measures. Maintaining good glycemic control is the most important preventive strategy, as elevated blood glucose levels create an environment conducive to Candida overgrowth. Patients should adhere to their prescribed tirzepatide regimen, monitor blood glucose as recommended, and work with their healthcare team to achieve individualized glycemic targets. The American Diabetes Association recommends an A1C goal of less than 7% for most adults with diabetes, though targets should be individualized based on patient factors. Regular follow-up appointments allow for medication adjustments and early identification of glycemic control issues.
Hygiene practices play a crucial role in preventing genitourinary fungal infections. Patients should be counseled to keep the genital area clean and dry, as moisture promotes fungal growth. Recommendations include wearing breathable cotton underwear, avoiding tight-fitting synthetic clothing, changing out of wet bathing suits or exercise clothing promptly, and avoiding douches or scented feminine hygiene products that can disrupt normal vaginal flora. After bathing, the genital area should be dried thoroughly. Women should wipe from front to back after using the toilet to prevent introducing intestinal flora to the vaginal area.
Dietary considerations may influence overall glycemic control, which indirectly affects infection risk. Following a balanced diet consistent with ADA nutrition recommendations can help maintain stable blood glucose levels. While some practitioners suggest limiting refined sugar and simple carbohydrates, the primary focus should be on overall glycemic management rather than specific anti-Candida dietary interventions, as evidence for the latter is limited.
The evidence for probiotic supplementation in preventing recurrent vulvovaginal candidiasis is insufficient, and probiotics are not routinely recommended by the CDC or Infectious Diseases Society of America for this purpose.
Patients experiencing recurrent yeast infections despite preventive measures should be referred for comprehensive evaluation, particularly if they have poorly controlled diabetes, are immunosuppressed, are pregnant, or have had multiple treatment failures. This may include assessment for inadequate diabetes control, immunosuppression, antibiotic use, hormonal factors, or resistant Candida species. In some cases, prophylactic antifungal therapy may be warranted. Healthcare providers should maintain open communication with patients about infection concerns and provide individualized prevention strategies based on patient-specific risk factors and preferences. Importantly, patients should be reassured that yeast infections, while uncomfortable, are treatable and that continuing tirzepatide therapy for diabetes management remains appropriate with proper preventive measures and prompt treatment of infections when they occur.
No, tirzepatide does not increase yeast infection risk. Unlike SGLT2 inhibitors that cause glucose in urine and promote fungal growth, tirzepatide improves blood sugar through insulin enhancement and glucagon suppression without causing glucosuria.
No, continue tirzepatide as prescribed during yeast infection treatment. Discontinuing the medication could worsen glycemic control and potentially increase infection susceptibility. Yeast infections are treatable with standard antifungal therapies while maintaining diabetes management.
Maintain optimal blood glucose control by adhering to your tirzepatide regimen and monitoring as recommended. Practice good hygiene including wearing breathable cotton underwear, keeping the genital area clean and dry, and avoiding tight synthetic clothing or scented products that disrupt normal flora.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.