LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Hashimoto's thyroiditis and tirzepatide represent an important intersection of autoimmune thyroid disease and modern metabolic therapy. Tirzepatide, a dual GIP/GLP-1 receptor agonist approved for type 2 diabetes and chronic weight management, offers significant benefits for patients struggling with metabolic challenges. Many individuals with Hashimoto's thyroiditis face weight gain and insulin resistance alongside thyroid dysfunction, making tirzepatide an attractive option. However, understanding potential interactions between tirzepatide and thyroid function, particularly regarding levothyroxine absorption and dosing adjustments, is essential for safe and effective treatment. This article examines the clinical considerations for patients with Hashimoto's thyroiditis considering or currently using tirzepatide.
Quick Answer: Patients with Hashimoto's thyroiditis can generally use tirzepatide for type 2 diabetes or weight management when appropriately indicated, though thyroid function monitoring and potential levothyroxine dose adjustments are necessary.
Patients with Hashimoto's thyroiditis often experience metabolic challenges that extend beyond thyroid dysfunction. Weight gain is a frequent concern, occurring both as a consequence of reduced metabolic rate and through interactions between thyroid hormones and insulin sensitivity. Research suggests an association between hypothyroidism and insulin resistance, though this relationship is complex and influenced by multiple factors. Some studies indicate that individuals with hypothyroidism may have an increased risk of metabolic syndrome and type 2 diabetes, though these associations are often confounded by other variables.
The relationship between thyroid function and glucose metabolism is bidirectional and clinically relevant. Thyroid hormones influence insulin secretion, glucose uptake in peripheral tissues, and hepatic glucose production. When thyroid hormone levels are inadequate, these processes may become altered, potentially contributing to glucose metabolism changes and weight management challenges. The inflammatory processes associated with autoimmune thyroiditis may also play a role in metabolic function, though more research is needed to fully characterize these relationships.
For patients with both Hashimoto's thyroiditis and type 2 diabetes or obesity, comprehensive metabolic management becomes essential. Treatment typically involves thyroid hormone replacement with levothyroxine to normalize thyroid function, alongside interventions targeting glycemic control and weight management. Understanding this metabolic interplay is important when considering newer therapeutic agents like tirzepatide for patients with coexisting autoimmune thyroid disease.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (under the brand name Mounjaro) and chronic weight management (under the brand name Zepbound). For weight management, Zepbound is indicated for adults with a BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related comorbid condition.
The mechanism of action involves activation of both GIP and GLP-1 receptors, which are expressed throughout the body including the pancreas, gastrointestinal tract, and central nervous system. GLP-1 receptor activation enhances glucose-dependent insulin secretion, suppresses inappropriate glucagon release, slows gastric emptying, and reduces appetite through central mechanisms. GIP receptor activation complements these effects by further enhancing insulin secretion and may have effects on lipid metabolism and energy expenditure, though the latter mechanisms are still being characterized in humans.
Clinical trials have demonstrated substantial efficacy for tirzepatide. In the SURPASS clinical trial program for type 2 diabetes, patients achieved HbA1c reductions of 1.9% to 2.6% depending on dose, with weight loss averaging 15-22 pounds across studies. In SURPASS-2, tirzepatide showed greater HbA1c and weight reductions compared to semaglutide 1 mg. The SURMOUNT trials evaluating tirzepatide for obesity showed weight reductions of 15-21% of body weight over 72 weeks at the highest doses.
Tirzepatide is administered as a once-weekly subcutaneous injection, with a recommended starting dose of 2.5 mg once weekly for 4 weeks, then increasing by 2.5 mg every 4 weeks until the target dose (up to 15 mg) is reached. Common adverse effects include gastrointestinal symptoms such as nausea, diarrhea, vomiting, and constipation, which are typically mild to moderate and often diminish over time. Important safety considerations include risks of pancreatitis, hypoglycemia (when used with insulin or insulin secretagogues), acute kidney injury from dehydration, and gallbladder disease. The medication carries a Boxed Warning regarding thyroid C-cell tumors based on rodent studies, though the clinical relevance to humans remains uncertain.
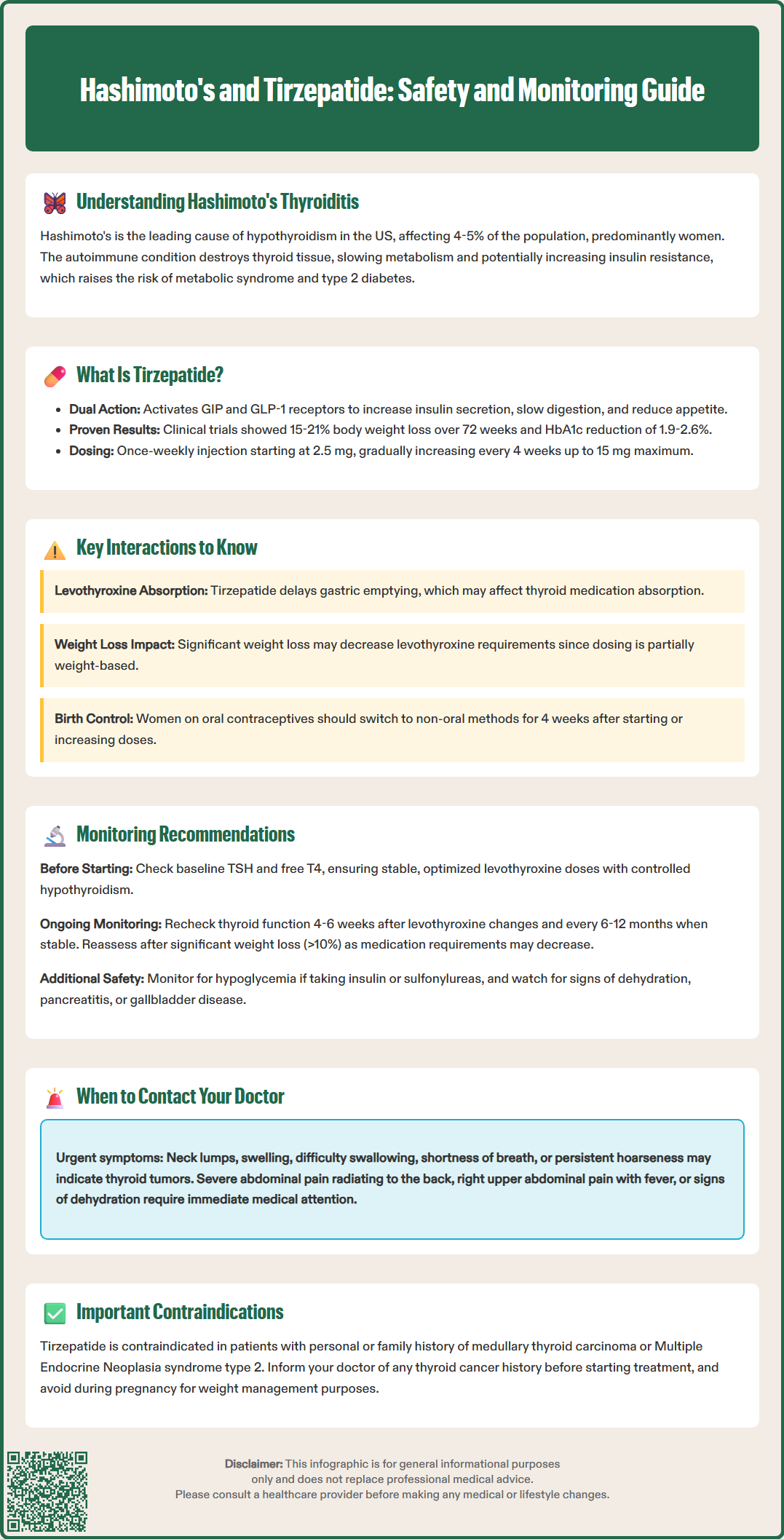
The relationship between tirzepatide and thyroid function in patients with Hashimoto's thyroiditis requires careful consideration. The primary thyroid-related concern with tirzepatide stems from preclinical rodent studies showing an increased incidence of thyroid C-cell tumors, leading to a Boxed Warning in the prescribing information. Tirzepatide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). However, there is no established link between GLP-1 or GIP receptor agonists and thyroid cancer in humans, and the relevance of rodent C-cell findings to human thyroid physiology remains questionable due to species differences in C-cell distribution and GLP-1 receptor expression.
For patients with Hashimoto's thyroiditis taking levothyroxine replacement therapy, an important consideration is tirzepatide's effect on gastric emptying, which may impact the absorption of oral medications. The FDA prescribing information notes that tirzepatide delays gastric emptying and has the potential to impact the absorption of oral medications, including those with narrow therapeutic indices like levothyroxine. Patients on levothyroxine should have thyroid function monitored after initiating tirzepatide and following dose increases, as adjustments to levothyroxine dosing may be necessary.
Tirzepatide may also reduce the efficacy of oral contraceptives. The FDA label recommends that women using oral hormonal contraceptives switch to a non-oral contraceptive method or add a barrier method for 4 weeks after initiation and for 4 weeks after each dose escalation of tirzepatide.
Weight loss induced by tirzepatide may indirectly affect levothyroxine dosing requirements. As body weight decreases, the dose of levothyroxine needed to maintain euthyroidism may also decrease, since thyroid hormone replacement is partially weight-based. Patients experiencing substantial weight loss should have thyroid function monitored to ensure their levothyroxine dose remains appropriate.
To date, there is no evidence that tirzepatide exacerbates autoimmune thyroid disease or increases thyroid antibody levels in patients with Hashimoto's thyroiditis, though specific studies in this population are limited. Patients with well-controlled Hashimoto's thyroiditis on stable levothyroxine therapy can generally be considered for tirzepatide treatment when indicated for type 2 diabetes or obesity management, with appropriate monitoring.
When prescribing tirzepatide to patients with Hashimoto's thyroiditis, several safety considerations warrant attention. The FDA-mandated Boxed Warning regarding thyroid C-cell tumors observed in rodent studies necessitates careful patient selection. Tirzepatide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Patients should be counseled about symptoms of thyroid tumors, including a neck mass, dysphagia, dyspnea, or persistent hoarseness, though routine calcitonin monitoring is not recommended for surveillance in the absence of specific risk factors.
Baseline thyroid function assessment is advisable before initiating tirzepatide in patients with known or suspected Hashimoto's thyroiditis. This should include measurement of thyroid-stimulating hormone (TSH) and, if not previously documented, free thyroxine (free T4) levels. Patients should be on a stable, optimized dose of levothyroxine before starting tirzepatide. For patients with uncontrolled hypothyroidism, thyroid hormone replacement should be optimized first, as untreated hypothyroidism can affect glucose metabolism and weight management outcomes.
Ongoing monitoring should include thyroid function testing at appropriate intervals, particularly in patients experiencing significant weight loss or after tirzepatide dose increases. The American Thyroid Association recommends checking TSH levels 4-6 weeks after any change in levothyroxine dose and then every 6-12 months once stable. For patients on tirzepatide who lose substantial weight (typically >10% of body weight), thyroid function should be reassessed as levothyroxine requirements may decrease.
Additional safety monitoring for tirzepatide includes:
Risk of hypoglycemia when used with insulin or insulin secretagogues (sulfonylureas); consider reducing doses of these medications when initiating tirzepatide
Signs of acute kidney injury, particularly in patients experiencing severe gastrointestinal adverse effects with dehydration
Symptoms of pancreatitis (severe abdominal pain radiating to the back, nausea, vomiting)
Gallbladder disease (right upper quadrant pain, fever, jaundice)
Gastrointestinal adverse effects, which occur commonly but are usually self-limited
Tirzepatide is not recommended for patients with severe gastrointestinal disease, including severe gastroparesis. It is contraindicated for weight management during pregnancy (Zepbound), and women of reproductive potential should be counseled about potential effects on oral contraceptive efficacy. Tirzepatide is not approved for use in patients under 18 years of age.
Patients with diabetic retinopathy should be monitored according to standard diabetes care guidelines, as rapid improvement in glycemic control has been associated with temporary worsening of retinopathy in some studies, though this is not a tirzepatide-specific labeled warning.
Patients with Hashimoto's thyroiditis considering or currently taking tirzepatide should maintain regular communication with their healthcare providers and understand specific circumstances requiring prompt medical attention. Immediate consultation is warranted if symptoms suggestive of thyroid tumors develop, including a lump or swelling in the neck, difficulty swallowing, shortness of breath, or persistent hoarseness. While the risk of medullary thyroid carcinoma in humans taking tirzepatide remains theoretical, these symptoms require urgent evaluation.
Changes in symptoms related to thyroid function should prompt contact with healthcare providers. If patients experience new or worsening symptoms of hypothyroidism—such as increased fatigue, cold intolerance, constipation, dry skin, or unexplained weight gain despite tirzepatide therapy—thyroid function testing may be needed to assess whether levothyroxine dose adjustment is required. Conversely, symptoms suggesting excessive thyroid hormone replacement (hyperthyroidism), including palpitations, tremor, anxiety, heat intolerance, or insomnia, particularly in the context of significant weight loss, warrant evaluation and possible levothyroxine dose reduction.
Patients should contact their healthcare provider for:
Symptoms of hypoglycemia (sweating, shakiness, dizziness, confusion, irritability) if taking tirzepatide with insulin or sulfonylureas
Severe or persistent gastrointestinal adverse effects, especially if unable to stay hydrated
Severe abdominal pain, especially if radiating to the back and accompanied by nausea and vomiting, which requires urgent evaluation to exclude pancreatitis
Right upper quadrant abdominal pain, fever, or yellowing of the skin or eyes, which may indicate gallbladder disease
Signs of dehydration or decreased kidney function (dizziness, decreased urination, extreme thirst)
Severe allergic reactions (rash, itching, swelling of face/throat, severe dizziness)
If pregnancy occurs or is planned, particularly for patients taking Zepbound for weight management
Patients should consult their healthcare provider before starting tirzepatide if they have a personal or family history of thyroid cancer, particularly medullary thyroid carcinoma, or Multiple Endocrine Neoplasia syndrome type 2. Women using oral contraceptives should discuss the need for alternative or additional contraceptive methods during tirzepatide initiation and dose escalation.
Regular follow-up appointments should be maintained to monitor weight loss progress, glycemic control (if diabetic), thyroid function, and overall tolerance of therapy. Collaborative care between primary care providers and endocrinology specialists often provides optimal management for patients with both Hashimoto's thyroiditis and metabolic conditions requiring tirzepatide therapy.
Yes, patients with well-controlled Hashimoto's thyroiditis on stable levothyroxine therapy can generally use tirzepatide when indicated for type 2 diabetes or obesity management. However, thyroid function should be monitored after starting tirzepatide and following dose increases, as the medication may affect levothyroxine absorption and weight loss may alter dosing requirements.
Tirzepatide delays gastric emptying and may impact the absorption of oral medications including levothyroxine. Patients taking levothyroxine should have thyroid function (TSH) monitored after initiating tirzepatide and following dose increases to determine if levothyroxine dose adjustments are needed.
Tirzepatide carries a Boxed Warning regarding thyroid C-cell tumors observed in rodent studies and is contraindicated in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. The clinical relevance to humans remains uncertain, and there is no established link between GLP-1 receptor agonists and thyroid cancer in humans.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.