LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Many patients taking semaglutide for diabetes management or weight loss wonder whether they can continue enjoying familiar snacks like popcorn. Semaglutide (Ozempic, Wegovy, Rybelsus) slows gastric emptying and reduces appetite, which can affect how your body tolerates different foods. While there are no official restrictions against eating popcorn during semaglutide treatment, individual tolerance varies based on portion size, preparation method, and your body's response to the medication. Understanding how semaglutide affects digestion helps you make informed choices about incorporating popcorn and other snacks into your eating plan while minimizing gastrointestinal discomfort and maintaining adequate nutrition.
Quick Answer: You can eat popcorn while taking semaglutide, as there are no official medical restrictions against it, though individual tolerance varies based on portion size and preparation method.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (under brand names Ozempic and Rybelsus) and chronic weight management (Wegovy). The medication works by mimicking the naturally occurring GLP-1 hormone, which regulates blood glucose and affects appetite through both central (brain) and peripheral mechanisms. Semaglutide slows gastric emptying—the rate at which food moves from your stomach into your small intestine—which contributes to increased satiety and reduced appetite, though this effect may diminish over time with continued treatment.
The delayed gastric emptying that contributes to semaglutide's effectiveness for weight loss means your digestive system processes food differently than before treatment. Many patients report feeling satisfied with smaller portion sizes and experiencing changes in food preferences. Some patients report developing aversions to previously enjoyed foods, particularly those high in fat or sugar, though individual experiences vary considerably.
Gastrointestinal side effects are among the most common experiences with semaglutide therapy. According to FDA prescribing information for Wegovy (semaglutide for weight management), nausea occurs in approximately 44% of patients, while vomiting (24%), diarrhea (30%), constipation (24%), and abdominal pain (20%) are also common. Rates are generally lower with Ozempic and Rybelsus at diabetes treatment doses. These effects are typically most pronounced during dose escalation and often improve with continued treatment.
Important safety information: Semaglutide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. It is not recommended for patients with severe gastroparesis. Understanding how semaglutide affects digestion helps patients make informed food choices that minimize discomfort while maintaining adequate nutrition. The medication does not prohibit specific foods, but individual tolerance may vary significantly.
There is no official contraindication or medical restriction against eating popcorn while taking semaglutide. The FDA-approved prescribing information for semaglutide products does not list popcorn or any specific foods as prohibited during treatment. Patients are generally advised to follow a balanced, reduced-calorie diet as recommended by their healthcare provider, but specific food restrictions are not mandated by the medication itself.
Popcorn can be compatible with semaglutide treatment when consumed mindfully and in appropriate portions. According to USDA FoodData Central, air-popped popcorn is a whole grain snack that provides dietary fiber—approximately 3.6 grams per 3-cup serving—which can be beneficial for digestive health and satiety. The fiber content may help with regularity, which is particularly relevant since constipation affects many semaglutide users. Plain popcorn is also relatively low in calories compared to many snack alternatives, with air-popped varieties containing roughly 93 calories per 3-cup serving.
However, individual tolerance is the key consideration. The delayed gastric emptying caused by semaglutide means that high-fiber or high-volume foods may sit in your stomach longer than usual. Some patients find that bulky foods like popcorn cause uncomfortable fullness, bloating, or abdominal distension, particularly when consumed in larger quantities. The experience varies considerably among individuals—some tolerate popcorn well, while others find it triggers gastrointestinal discomfort.
The preparation method significantly impacts how well popcorn fits into a semaglutide-compatible eating pattern. Air-popped or lightly seasoned popcorn is generally better tolerated than varieties heavily coated with butter, oil, cheese, or caramel, as high-fat additions may exacerbate nausea or delayed digestion. Patients with significant gastroparesis symptoms or severe gastrointestinal effects from semaglutide should be particularly cautious with high-residue foods like popcorn and may need to consult their healthcare provider about dietary modifications.
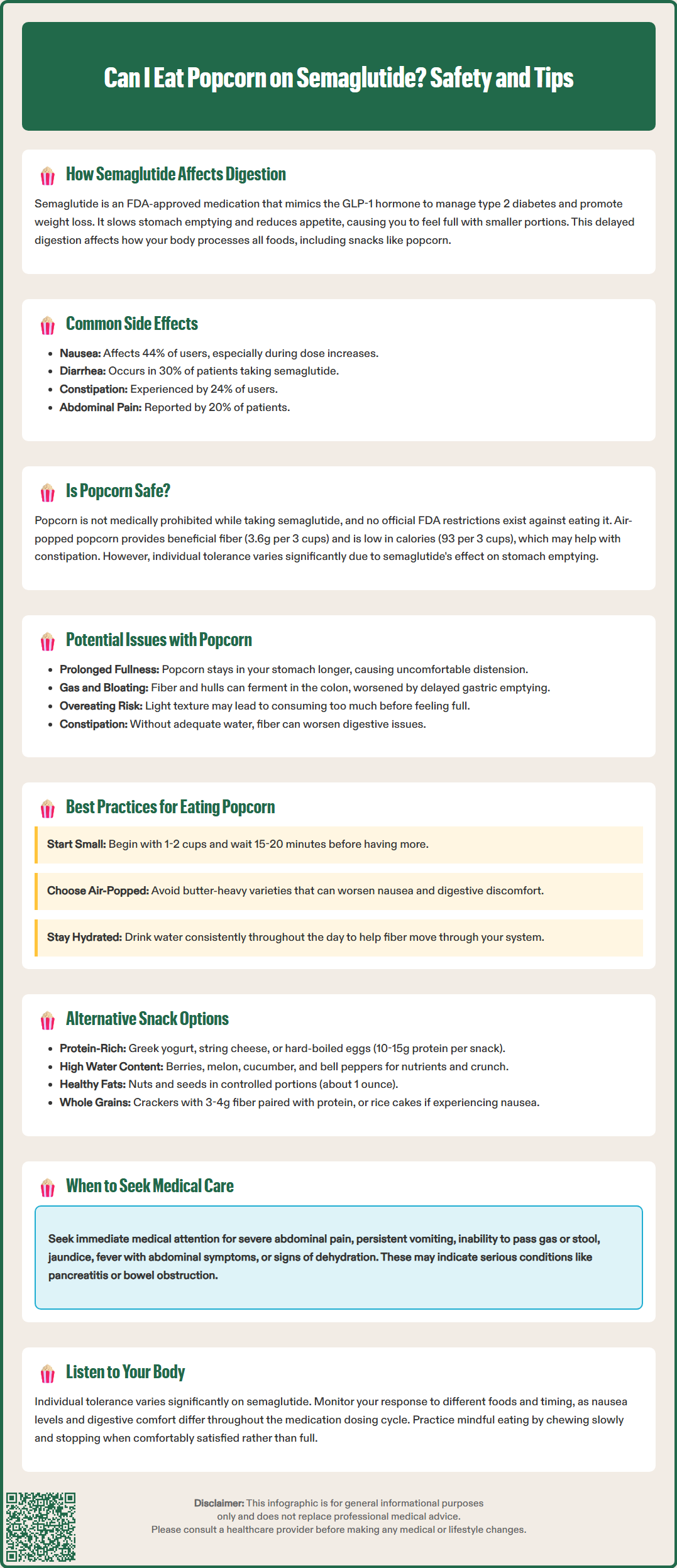
While popcorn itself does not interact pharmacologically with semaglutide, the combination of this high-fiber, high-volume food with the medication's effects on gastric emptying can produce uncomfortable symptoms in some individuals. The most commonly reported issue is prolonged fullness or a sensation of excessive abdominal distension. Because semaglutide slows the movement of food through your digestive tract, a serving of popcorn that would normally digest relatively quickly may remain in your stomach for an extended period, creating persistent feelings of fullness that some patients describe as uncomfortable.
Bloating and gas are potential concerns when consuming popcorn during semaglutide treatment. Popcorn is a whole grain containing both soluble and insoluble fiber, and the hulls (the hard outer shells) can be particularly difficult to digest. When these components reach the colon, they undergo bacterial fermentation, potentially producing increased intestinal gas. This process, combined with delayed gastric emptying from semaglutide, may lead to more pronounced or prolonged bloating symptoms in some patients.
Nausea represents another consideration, though this is more likely related to portion size and preparation method than to popcorn specifically. Eating any food too quickly or in excessive amounts while on semaglutide can trigger or worsen nausea. Popcorn's light, airy texture may lead some people to consume larger volumes than they realize, only to experience delayed-onset nausea as the food accumulates in the stomach. Additionally, heavily buttered or flavored popcorn introduces fats that can intensify nausea in semaglutide users.
Constipation, while seemingly counterintuitive given popcorn's fiber content, can occur if popcorn is consumed without adequate fluid intake. Fiber requires sufficient hydration to move effectively through the intestinal tract.
When to seek medical care: Contact your healthcare provider promptly if you experience severe or persistent abdominal pain, pain that radiates to your back, persistent vomiting, inability to pass gas or stool, yellowing of skin/eyes, fever with abdominal symptoms, or signs of dehydration. These could indicate serious conditions such as pancreatitis, gallbladder disease, bowel obstruction, or severe gastroparesis that require immediate medical attention.
Successful snacking during semaglutide therapy requires a strategic approach that accounts for the medication's effects on appetite and digestion. Portion control is paramount—even with healthy snacks like popcorn. Start with smaller servings than you might have consumed before treatment, such as 1-2 cups of popped popcorn rather than a full bowl. The delayed gastric emptying means you may not feel full immediately after eating, so consuming food slowly and waiting 15-20 minutes before deciding whether to eat more can prevent uncomfortable overfullness.
Timing matters significantly when planning snacks. Many patients find that eating smaller, more frequent meals and snacks works better than traditional three-meal patterns while on semaglutide. For patients experiencing significant gastroparesis symptoms, spacing meals and snacks by several hours may help improve tolerance. This approach allows adequate time for gastric emptying between eating occasions. Additionally, some patients report varying levels of nausea throughout their dosing cycle, though experiences differ considerably among individuals.
Preparation methods dramatically influence tolerability. For popcorn specifically, choose air-popped varieties or those prepared with minimal added fat. Avoid movie theater-style popcorn with heavy butter or oil, as well as pre-packaged microwave varieties that often contain significant amounts of fat, sodium, and artificial flavorings. Light seasoning with herbs, nutritional yeast, or a small amount of salt is generally better tolerated than rich, creamy, or sweet coatings.
Hydration is essential throughout semaglutide treatment and particularly important when consuming fiber-rich snacks. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), drinking plenty of water and other fluids helps prevent constipation when increasing fiber intake. Drink water consistently throughout the day rather than consuming large amounts with meals, which can contribute to uncomfortable fullness. Keep a water bottle accessible and aim for steady hydration rather than drinking large volumes at once.
Patients seeking snack alternatives to popcorn while on semaglutide should focus on options that provide nutritional value without triggering gastrointestinal discomfort. Protein-rich snacks are often well-tolerated and support satiety without excessive volume. Greek yogurt (plain or lightly sweetened), string cheese, hard-boiled eggs, or small portions of lean deli meat provide protein that helps maintain muscle mass during weight loss. While protein generally has less impact on blood glucose than carbohydrates, individual responses vary, and larger amounts of protein can affect blood glucose in some people, particularly those with diabetes. A practical target of 10-15 grams of protein per snack provides satiety benefits for many patients.
Fresh fruits and vegetables offer vitamins, minerals, and fiber with high water content that many patients tolerate well. Berries, melon, cucumber slices, cherry tomatoes, and bell pepper strips provide satisfying crunch and natural sweetness without the bulk of popcorn. Pairing vegetables with a small amount of hummus or guacamole adds healthy fats and protein. Some patients may find that dried fruits, which are calorie-dense and contain concentrated fiber and sugar, can cause digestive discomfort; starting with small test portions is advisable.
Nuts and seeds in controlled portions provide healthy fats, protein, and fiber. A small handful (approximately 1 ounce) of almonds, walnuts, or pumpkin seeds offers sustained energy and satisfaction. These foods are nutrient-dense, so portion control is essential—pre-portioning into small containers or bags can prevent overconsumption. Nut butters spread on apple slices or whole grain crackers provide similar benefits with added variety.
Whole grain crackers with minimal added fat can satisfy the desire for something crunchy without the volume of popcorn. Look for options with 3-4 grams of fiber per serving and pair with protein sources like low-fat cheese or turkey slices. Rice cakes, while less nutritionally dense, are light and often well-tolerated by patients experiencing nausea.
Regardless of snack choice, mindful eating practices enhance tolerance and satisfaction during semaglutide treatment. Eat slowly, chew thoroughly, and pay attention to satiety signals. Stop eating when comfortably satisfied rather than completely full, as the delayed feedback from your digestive system means you may feel increasingly uncomfortable 20-30 minutes after finishing a snack. If you experience persistent gastrointestinal symptoms that interfere with adequate nutrition, consult your healthcare provider for personalized dietary guidance.
No, FDA prescribing information for semaglutide does not prohibit specific foods. Patients are advised to follow a balanced, reduced-calorie diet, but individual tolerance to different foods varies based on how the medication affects gastric emptying and digestion.
Semaglutide slows gastric emptying, causing high-fiber, high-volume foods like popcorn to remain in the stomach longer than usual. This can lead to prolonged fullness, bloating, or gas, particularly when consumed in large portions or with heavy butter or oil.
Start with small portions (1-2 cups), choose air-popped or lightly seasoned varieties, eat slowly, and maintain adequate hydration. Avoid heavily buttered or high-fat preparations that may worsen nausea or digestive discomfort.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.