LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Can you drink alcohol with weight loss injections? This common question arises for many patients prescribed GLP-1 medications like semaglutide (Wegovy) or tirzepatide (Zepbound). While there is no absolute prohibition against alcohol consumption with these FDA-approved weight loss medications, the combination requires careful consideration. Alcohol can interfere with treatment effectiveness, worsen gastrointestinal side effects, and pose specific risks for patients with diabetes. Understanding how these medications interact with alcohol helps you make informed decisions that support your weight loss goals while minimizing potential complications. This guide provides evidence-based recommendations for safe alcohol use during treatment.
Quick Answer: There is no absolute prohibition against drinking alcohol with weight loss injections, but alcohol can reduce treatment effectiveness, worsen side effects, and increase risks like hypoglycemia.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections approved by the FDA for chronic weight management include semaglutide (Wegovy) and tirzepatide (Zepbound). These medications work through different but related mechanisms—semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist, while tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist. Note that Ozempic (semaglutide) and Mounjaro (tirzepatide) are FDA-approved for type 2 diabetes management, with any weight loss use being off-label.
These medications primarily work by binding to receptors in the brain that control appetite and satiety, significantly reducing hunger signals and increasing feelings of fullness after eating smaller portions. Additionally, they slow gastric emptying—the rate at which food leaves your stomach—which prolongs the sensation of fullness and helps reduce overall caloric intake.
Beyond appetite suppression, these medications enhance insulin secretion in response to elevated blood glucose while suppressing glucagon release. This helps stabilize blood sugar levels and improves metabolic function. The medications are administered via subcutaneous injection, typically once weekly, allowing for sustained therapeutic effects.
Clinical trials have demonstrated significant efficacy, with patients losing approximately 15% of body weight with semaglutide 2.4 mg (STEP 1 trial) and up to 20% with tirzepatide (SURMOUNT-1 trial) when combined with lifestyle modifications. These medications are generally prescribed for adults with a body mass index (BMI) of 30 kg/m² or greater, or 27 kg/m² or greater with at least one weight-related comorbidity such as type 2 diabetes or hypertension. Understanding how these medications function is essential when considering potential interactions with substances like alcohol.
There is no official contraindication or absolute prohibition against consuming alcohol while using GLP-1 or GIP/GLP-1 receptor agonist weight loss injections. The FDA prescribing information for medications like semaglutide and tirzepatide does not list alcohol as a specific drug interaction or require complete abstinence. However, this absence of a formal warning does not mean that combining alcohol with these medications is without considerations or potential complications.
Alcohol consumption can significantly impact the effectiveness of your weight loss treatment. Alcoholic beverages are calorie-dense, with each gram of alcohol providing approximately 7 calories—nearly as much as fat. Regular or excessive drinking can substantially increase your daily caloric intake, potentially offsetting the appetite-suppressing benefits of your weight loss medication. Mixed drinks, cocktails, and beer often contain additional sugars and carbohydrates that further contribute to caloric excess.
The gastrointestinal effects of these medications may interact with alcohol consumption. Since these injections slow gastric emptying, alcohol may be absorbed more slowly than usual, which could delay the onset of alcohol effects and potentially lead to inadvertent overconsumption. This delayed absorption, combined with the medications' known side effects, may increase the likelihood of nausea, vomiting, or abdominal discomfort. Some patients anecdotally report altered responses to alcohol while taking these medications, though individual experiences vary considerably.
Preliminary research suggests that GLP-1 receptor agonists may reduce alcohol cravings and consumption in some individuals, though this effect varies between patients. While this potential benefit is being investigated, it should not be considered a primary reason for using these medications, which are specifically FDA-indicated for weight management and/or glycemic control in appropriate patients.
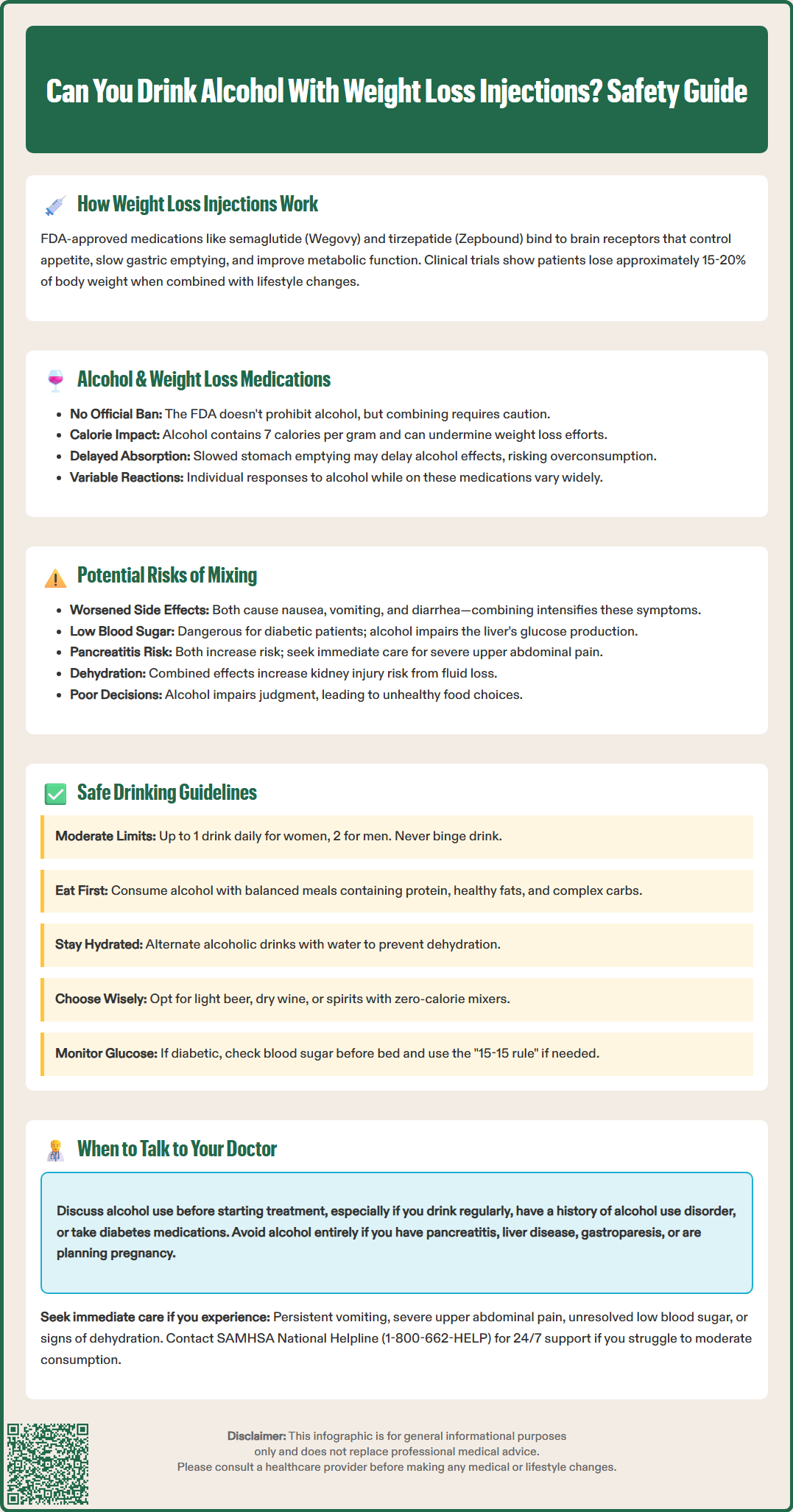
Combining alcohol with weight loss injections carries several clinically relevant risks that warrant careful consideration. The most common concern involves exacerbation of gastrointestinal side effects. GLP-1 and GIP/GLP-1 receptor agonists frequently cause nausea, vomiting, diarrhea, and abdominal discomfort, particularly during dose escalation. Alcohol is independently associated with gastric irritation and can trigger or worsen these symptoms, potentially leading to dehydration, electrolyte imbalances, and reduced medication adherence.
Hypoglycemia represents a more serious potential complication, particularly for patients with diabetes. While these medications have a relatively low intrinsic risk of causing dangerously low blood sugar when used alone, the risk increases significantly when combined with insulin or sulfonylureas. Alcohol consumption can impair the liver's ability to produce glucose through gluconeogenesis, especially during fasting states or several hours after drinking. This effect, combined with glucose-lowering medications, can result in symptomatic hypoglycemia characterized by shakiness, confusion, sweating, and in severe cases, loss of consciousness. Patients with diabetes should check blood glucose before bed after drinking and consider having a snack containing carbohydrates to reduce overnight hypoglycemia risk.
Pancreatitis, though rare, is a recognized adverse effect of these medications. Excessive alcohol consumption is also an independent risk factor for both acute and chronic pancreatitis. If you experience severe upper abdominal pain radiating to the back, especially with nausea or vomiting, stop taking your weight loss medication immediately and seek urgent medical care. These symptoms could indicate pancreatitis requiring prompt evaluation.
Additionally, the combination of alcohol-induced dehydration and medication-related gastrointestinal effects may increase the risk of acute kidney injury. Persistent vomiting, diarrhea, or inability to maintain adequate fluid intake warrants medical attention. Finally, alcohol's effects on judgment may undermine the behavioral modifications essential for successful weight loss, leading to poor food choices and reduced physical activity.
If you choose to consume alcohol while using weight loss injections, following evidence-based guidelines can help minimize potential risks. The Dietary Guidelines for Americans 2020-2025 and the CDC define moderate drinking as up to one drink per day for women and up to two drinks per day for men. One standard drink is defined as 12 ounces of beer (5% alcohol), 5 ounces of wine (12% alcohol), or 1.5 ounces of distilled spirits (40% alcohol). It's important to note that these guidelines are not recommendations to start drinking for health benefits.
Avoid binge drinking, defined by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) as consuming 4 or more drinks for women or 5 or more drinks for men on a single occasion. Binge drinking can significantly increase risks of medication side effects and may counteract weight loss efforts.
Timing your alcohol consumption strategically may reduce gastrointestinal discomfort. Avoid drinking on an empty stomach, as this can worsen medication-related nausea. Consuming alcohol with a balanced meal that includes protein, healthy fats, and complex carbohydrates can slow absorption and minimize adverse effects. Stay well-hydrated by alternating alcoholic beverages with water, which helps prevent dehydration that may worsen nausea or contribute to headaches.
Choose lower-calorie alcoholic options to support your weight loss goals. Light beer, dry wines, and spirits mixed with zero-calorie beverages (such as vodka with soda water and lime) provide fewer calories than sugary cocktails, regular beer, or sweet wines. Be mindful of portion sizes, as restaurant and home pours often exceed standard drink measurements.
For people with diabetes, additional precautions are necessary. Check your blood glucose before bed after drinking alcohol, carry fast-acting carbohydrates (like glucose tablets), and follow the "15-15 rule" if hypoglycemia occurs: consume 15 grams of carbohydrates, wait 15 minutes, and recheck blood glucose. Consider using continuous glucose monitoring if available, and ensure someone knows you have diabetes if drinking socially.
Open communication with your healthcare provider about alcohol consumption is essential for safe and effective weight loss treatment. Schedule a discussion before starting weight loss injections if you regularly consume alcohol, have a history of alcohol use disorder, or have concerns about how drinking might affect your treatment. Your doctor can provide personalized guidance based on your complete medical history, current medications, and individual risk factors.
Certain medical conditions warrant particular caution or may necessitate alcohol abstinence while using these medications. Contact your physician if you have a history of pancreatitis, liver disease, gastroparesis, or severe gastrointestinal disorders. Patients with type 2 diabetes require individualized counseling about hypoglycemia risk, especially if taking additional glucose-lowering medications such as insulin or sulfonylureas. Those with a history of alcohol dependence should discuss whether weight loss injections are appropriate and receive support for maintaining sobriety.
If you're planning a pregnancy, discuss this with your healthcare provider, as alcohol should be avoided during pregnancy, and medications like semaglutide should be discontinued at least 2 months before a planned pregnancy according to FDA labeling.
Seek immediate medical attention and stop your weight loss medication if you experience severe symptoms after combining alcohol with your medication. Warning signs requiring urgent evaluation include persistent vomiting that prevents fluid intake, severe upper abdominal pain (particularly if radiating to the back), signs of hypoglycemia that don't resolve with carbohydrate intake, symptoms of dehydration (decreased urination, extreme thirst, dizziness), or any other concerning reactions.
If you find it difficult to moderate alcohol intake, resources are available. The SAMHSA National Helpline (1-800-662-HELP) provides 24/7 treatment referral services. Regular follow-up appointments provide opportunities to reassess your alcohol consumption patterns and their impact on treatment outcomes. Be honest about your drinking habits, as this information helps your healthcare team optimize your weight loss plan and identify potential barriers to success.
Alcohol doesn't stop weight loss injections from working, but it can significantly reduce their effectiveness. Alcoholic beverages are calorie-dense, providing approximately 7 calories per gram, which can offset the caloric deficit created by appetite suppression and potentially slow your weight loss progress.
Alcohol can increase hypoglycemia risk, particularly for patients with diabetes taking additional glucose-lowering medications like insulin or sulfonylureas. Alcohol impairs the liver's ability to produce glucose, especially several hours after drinking, which can lead to dangerously low blood sugar levels requiring monitoring and precautions.
There is no specific waiting period required after administering your weight loss injection before consuming alcohol. However, if you experience gastrointestinal side effects during dose escalation, it may be prudent to avoid alcohol until these symptoms stabilize, and always follow moderate drinking guidelines when you do consume alcohol.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.