LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist that effectively suppresses appetite in most patients. However, some individuals report experiencing sweet cravings during treatment, which may seem counterintuitive given the medication's appetite-reducing effects. Understanding why these cravings occur and how to manage them is essential for optimizing treatment outcomes. This article explores the mechanisms behind sweet cravings on tirzepatide, evidence-based management strategies, and when to seek medical guidance to ensure safe, effective diabetes management and weight control.
Quick Answer: Some patients experience sweet cravings on tirzepatide despite its appetite-suppressing effects, potentially due to compensatory eating patterns, blood sugar fluctuations, or psychological factors.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). The medication works by mimicking naturally occurring incretin hormones that regulate blood sugar and appetite through multiple mechanisms.
The appetite-suppressing effects of tirzepatide occur through several pathways. GLP-1 receptor activation in the hypothalamus reduces hunger signals and increases satiety, while delayed gastric emptying prolongs the feeling of fullness after meals. Tirzepatide may also influence reward pathways in the brain that govern food preferences and eating behaviors. Clinical trials have demonstrated reductions in overall caloric intake among many patients taking tirzepatide.
Many patients experience a reduction in appetite during the first few weeks of treatment. This effect may change as the dose is gradually increased according to the FDA-approved schedule (typically starting at 2.5 mg weekly and increasing stepwise as tolerated). The medication's impact on food cravings appears to vary between individuals, with some patients reporting changes in preferences for certain foods. Individual responses vary considerably, and the relationship between tirzepatide and specific food cravings continues to be observed in clinical practice.
While tirzepatide generally suppresses appetite, some patients report persistent or even increased cravings for sweets during treatment. There is no official FDA-recognized link between tirzepatide and increased sweet cravings, but several possible mechanisms might explain this phenomenon in some individuals.
Blood sugar fluctuations may also contribute to sweet cravings in some patients. While tirzepatide improves overall glycemic control, patients who experience periods of relative hypoglycemia may develop physiological cravings for quick-acting carbohydrates. This is especially relevant for patients taking tirzepatide alongside insulin or sulfonylureas, which can increase hypoglycemia risk. Blood glucose monitoring is particularly important during dose adjustments for these patients.
Psychological factors should not be overlooked. Food restriction, even when appetite is pharmacologically reduced, can trigger psychological cravings for certain foods. Patients who previously relied on food for emotional regulation may find that as their overall appetite decreases, specific cravings for comfort foods—often sweets—become more noticeable.
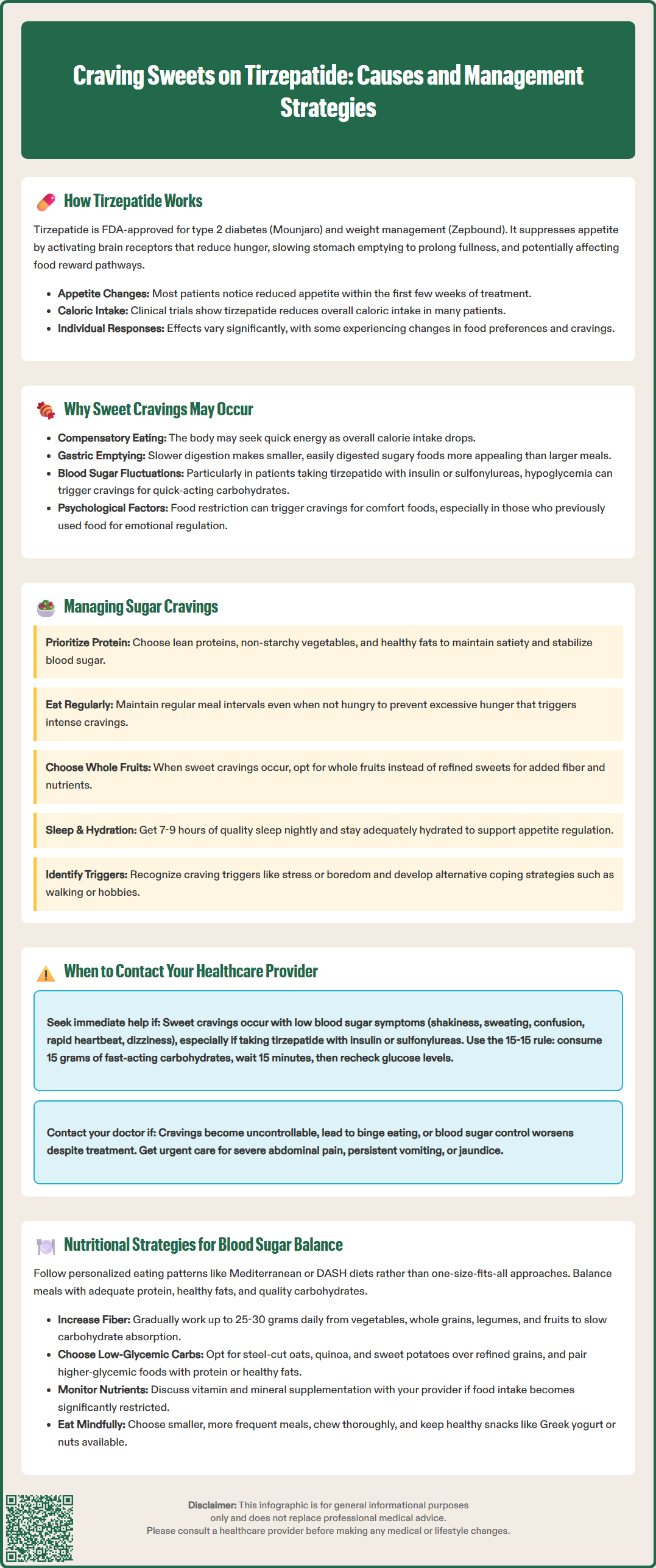
Effective management of sweet cravings on tirzepatide requires a balanced approach that addresses both physiological needs and behavioral patterns. The goal is to maintain the medication's therapeutic benefits while preventing counterproductive eating habits that could undermine metabolic improvements.
Dietary strategies form the foundation of craving management. Ensuring adequate protein intake at meals helps maintain satiety and stabilize blood sugar levels. The American Diabetes Association (ADA) recommends individualized nutrition therapy rather than fixed macronutrient distributions. Patients should prioritize nutrient-dense foods despite reduced appetite, focusing on lean proteins, non-starchy vegetables, and healthy fats. When sweet cravings occur, choosing whole fruits provides natural sugars along with fiber, vitamins, and minerals that refined sweets lack.
Meal timing and structure play crucial roles. Eating at regular intervals, even when appetite is diminished, prevents excessive hunger that can trigger intense cravings. Meal patterns should be individualized based on tolerance and blood glucose response, particularly for patients also taking insulin or sulfonylureas. For hypoglycemia (blood glucose below 70 mg/dL), the ADA recommends the 15-15 rule: consume 15 grams of fast-acting carbohydrates, wait 15 minutes, and recheck blood glucose.
Hydration and sleep are important factors. Maintaining adequate hydration based on individual needs and health status is essential, with requirements varying based on activity level and medical conditions. Poor sleep quality disrupts hormones that regulate appetite and cravings. The American Academy of Sleep Medicine recommends 7-9 hours of quality sleep nightly for most adults.
Behavioral modifications include identifying triggers for sweet cravings, such as stress, boredom, or specific times of day. Developing alternative coping strategies—walking, calling a friend, or engaging in a hobby—can interrupt automatic eating patterns. Mindful eating practices, where patients eat slowly and without distractions, enhance awareness of true hunger versus habitual or emotional eating.
While occasional sweet cravings on tirzepatide are generally not concerning, certain patterns warrant medical evaluation. Patients should contact their healthcare provider if cravings significantly interfere with diabetes management or weight loss goals, or if they indicate underlying metabolic issues.
Immediate consultation is recommended if sweet cravings are accompanied by symptoms of hypoglycemia, including shakiness, sweating, confusion, rapid heartbeat, or dizziness. This is particularly important for patients taking tirzepatide alongside sulfonylureas or insulin, as dose adjustments of these medications may be necessary. The American Diabetes Association recommends treating blood glucose levels below 70 mg/dL promptly with 15 grams of fast-acting carbohydrate, rechecking after 15 minutes, and repeating if necessary. Recurrent episodes require medication review.
Patients should also seek guidance if they experience uncontrollable cravings that lead to binge eating episodes or if they consume large quantities of sweets despite feeling physically full. This pattern may indicate that psychological factors require additional support. Referral to a registered dietitian or behavioral health specialist may be appropriate.
Worsening glycemic control despite tirzepatide treatment, evidenced by rising fasting glucose or HbA1c levels, necessitates provider contact. If sweet cravings are leading to significant carbohydrate consumption that counteracts the medication's glucose-lowering effects, treatment adjustments or additional interventions may be needed.
Urgent medical attention is needed for severe abdominal pain (which could indicate pancreatitis), persistent vomiting leading to dehydration, or symptoms of gallbladder disease such as right upper quadrant pain or jaundice, as these are potential serious adverse effects of tirzepatide.
Finally, patients should discuss cravings during routine follow-up appointments, particularly if they notice patterns related to dose escalation or if cravings persist beyond the initial adjustment period. Documentation of food intake, craving patterns, and blood glucose readings helps providers make informed recommendations.
Optimizing nutrition while taking tirzepatide enhances the medication's metabolic benefits and minimizes problematic cravings. A structured approach to meal planning supports stable blood glucose levels and sustainable weight management.
Macronutrient balance is fundamental. The American Diabetes Association recommends individualized eating patterns rather than a single ideal macronutrient distribution. Options include Mediterranean, DASH, or moderately low-carbohydrate approaches based on personal preferences and metabolic goals. Despite reduced appetite, patients should aim for balanced meals containing adequate protein, healthy fats, and quality carbohydrates. Protein sources should include lean meats, fish, eggs, legumes, and low-fat dairy products as appropriate for individual health needs.
Fiber intake deserves special attention. According to U.S. Dietary Guidelines, adults should aim for 25-30 grams of fiber daily from vegetables, whole grains, legumes, and fruits. Fiber slows carbohydrate absorption and enhances satiety. Patients should increase fiber gradually to minimize gastrointestinal discomfort, which can be more pronounced with tirzepatide's delayed gastric emptying.
Glycemic index considerations help maintain stable blood sugar. Choosing lower-glycemic carbohydrates—such as steel-cut oats, quinoa, sweet potatoes, and non-starchy vegetables—over refined grains and sugars prevents rapid glucose spikes and subsequent crashes that might intensify cravings. When consuming higher-glycemic foods, pairing them with protein or healthy fats can moderate their glycemic impact.
Micronutrient adequacy becomes challenging when appetite is suppressed. Patients with significantly restricted food intake may consider discussing vitamin and mineral supplementation with their healthcare provider. Regular monitoring of nutritional status may be warranted for patients with substantial dietary restrictions.
Practical meal planning should accommodate tirzepatide's gastrointestinal effects. Smaller, more frequent meals are often better tolerated than large portions for some patients. Eating slowly, chewing thoroughly, and stopping when comfortably satisfied rather than full may help manage gastrointestinal symptoms. Keeping healthy snacks available—such as Greek yogurt, nuts, or vegetable sticks with hummus—provides alternatives when sweet cravings emerge. Working with a registered dietitian nutritionist (RDN), particularly one familiar with diabetes care, can provide personalized guidance that aligns nutritional strategies with individual metabolic needs and treatment goals.
While tirzepatide typically suppresses appetite, some patients do experience sweet cravings due to compensatory eating patterns, blood sugar fluctuations, or psychological factors. Individual responses vary considerably, and these cravings can be managed through dietary strategies and behavioral modifications.
Tirzepatide alone has low hypoglycemia risk, but patients taking it alongside insulin or sulfonylureas may experience blood sugar drops that trigger physiological cravings for quick-acting carbohydrates. Blood glucose monitoring is particularly important during dose adjustments for these patients.
Contact your healthcare provider if cravings are accompanied by hypoglycemia symptoms (shakiness, sweating, confusion), lead to uncontrollable eating episodes, or result in worsening blood sugar control despite treatment. Immediate medical attention is needed for severe abdominal pain, persistent vomiting, or signs of gallbladder disease.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.