LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

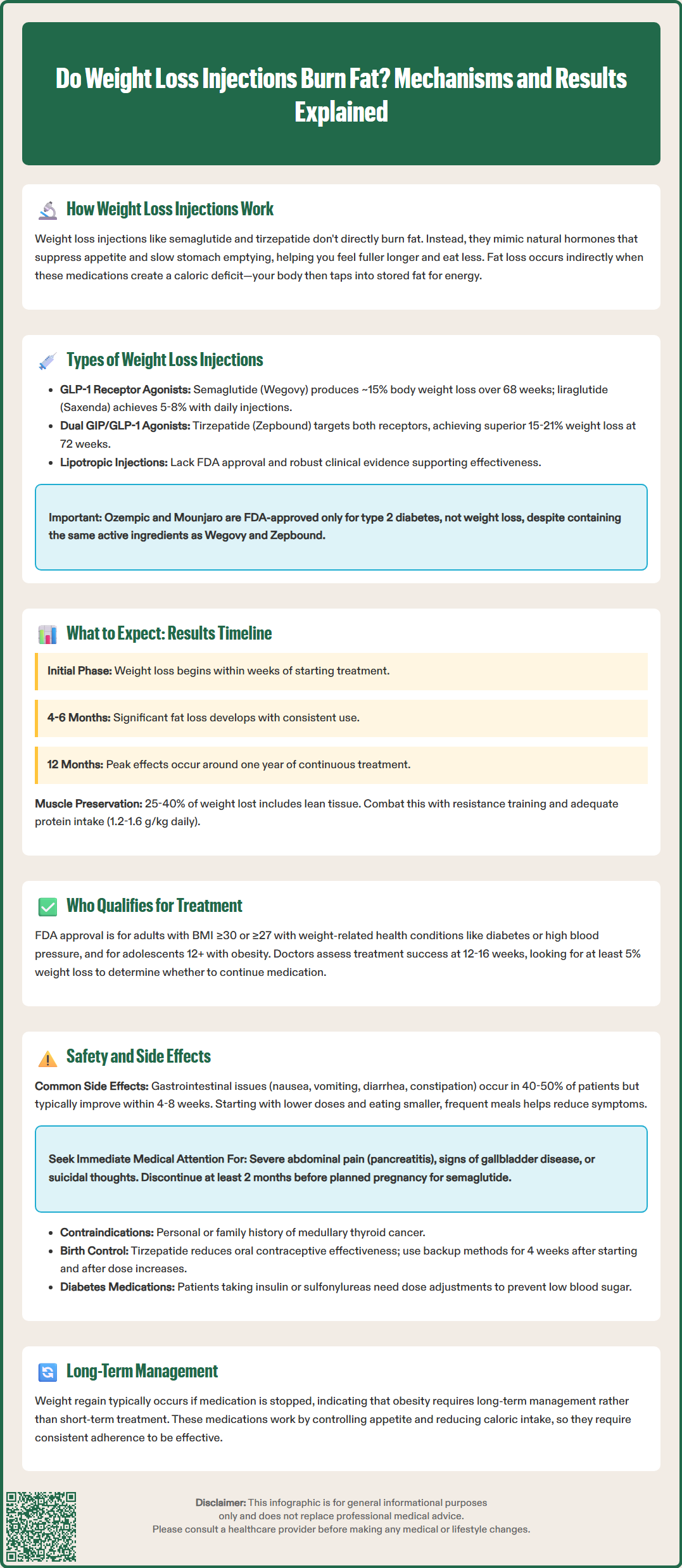
Weight loss injections have become increasingly popular for obesity management, but many patients wonder whether these medications directly burn fat. Understanding how these FDA-approved treatments work is essential for setting realistic expectations. Rather than acting as traditional fat burners, medications like semaglutide (Wegovy), liraglutide (Saxenda), and tirzepatide (Zepbound) work primarily through appetite suppression and metabolic regulation. This article explains the mechanisms behind weight loss injections, clarifies the difference between fat burning and fat loss, and provides evidence-based information on what patients can expect from these treatments.
Quick Answer: Weight loss injections do not directly burn fat but instead work through appetite suppression and metabolic regulation, creating a caloric deficit that leads to gradual fat loss over time.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections do not directly burn fat in the traditional sense of increasing metabolic fat oxidation. Instead, these medications work primarily through appetite suppression and metabolic regulation, which indirectly leads to fat loss over time through sustained caloric deficit.
The most commonly prescribed weight loss injections include glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), as well as tirzepatide (Zepbound), which is a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist. These medications mimic naturally occurring hormones that regulate blood sugar and appetite. When administered, they bind to receptors in the brain, particularly in areas controlling hunger and satiety, leading to reduced food intake and increased feelings of fullness after smaller meals.
Additionally, these injections slow gastric emptying, meaning food remains in the stomach longer, prolonging satiety between meals. This mechanism does not accelerate fat breakdown (lipolysis) directly but creates the physiological conditions necessary for the body to utilize stored fat as energy. When caloric intake decreases below energy expenditure, the body mobilizes adipose tissue for fuel, resulting in gradual fat loss.
These medications may also improve insulin sensitivity and glucose metabolism, primarily as a result of weight loss, which can indirectly support fat loss by reducing insulin resistance—a condition that promotes fat storage. FDA-approved weight management injections are indicated for adults with a BMI ≥30 kg/m² (obesity) or ≥27 kg/m² with at least one weight-related comorbidity (such as hypertension, type 2 diabetes, or dyslipidemia). Wegovy is also approved for weight management in adolescents aged 12 and older with obesity.
Several categories of weight loss injections are available, each with distinct mechanisms of action. Understanding these differences helps clarify how they contribute to fat loss.
GLP-1 Receptor Agonists represent a major class of FDA-approved weight management medications. Semaglutide (Wegovy) works by activating GLP-1 receptors, reducing appetite, slowing gastric emptying, and improving glycemic control. The STEP 1 clinical trial demonstrated average weight loss of approximately 15% of body weight over 68 weeks when combined with lifestyle interventions. Liraglutide (Saxenda) operates similarly but requires daily injections and typically produces more modest weight loss of approximately 5-8% of body weight in the SCALE clinical program.
Dual GIP/GLP-1 Receptor Agonists like tirzepatide (Zepbound) represent a newer approach, targeting both glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptors. This dual mechanism enhances metabolic effects, with the SURMOUNT-1 trial showing dose-dependent weight loss ranging from approximately 15% to 21% of body weight at 72 weeks, with the highest dose achieving the greatest effect. The contribution of GIP receptor activation to weight loss is still being studied, though it appears to enhance the effects beyond GLP-1 action alone.
Lipotropic Injections containing compounds like methionine, inositol, choline, and vitamin B12 are sometimes marketed for weight loss, though there is no robust clinical evidence supporting their efficacy for fat burning or significant weight reduction. These are not FDA-approved for weight management and lack the rigorous safety and effectiveness data of prescription medications.
The American Diabetes Association, American College of Physicians, and American Gastroenterological Association recognize GLP-1 receptor agonists and dual GIP/GLP-1 receptor agonists as evidence-based options for weight management in appropriate patients, particularly those with obesity and related comorbidities. It's important to note that medications like Ozempic (semaglutide) and Mounjaro (tirzepatide) are FDA-approved only for type 2 diabetes management, not for weight loss, though they contain the same active ingredients as their weight management counterparts.
Understanding the distinction between fat loss and overall weight loss is crucial when considering weight loss injections. While these medications effectively reduce body weight, not all weight lost represents fat tissue.
Clinical studies of GLP-1 receptor agonists and dual GIP/GLP-1 receptor agonists demonstrate that a majority of weight lost consists of fat mass, with the remainder comprising lean tissue, including muscle and water. This ratio is actually favorable compared to rapid weight loss through extreme caloric restriction alone, which often results in greater muscle loss. However, preserving lean body mass remains important for maintaining metabolic rate and functional capacity.
Patients typically observe gradual weight reduction beginning within the first few weeks of treatment, with significant effects developing over months and peak effects occurring around one year of continuous use. Initial weight loss may include water weight as dietary sodium intake decreases with reduced food consumption. Fat loss becomes more apparent over subsequent months as the body adapts to sustained caloric deficit.
Expected timeline for results:
First 12-16 weeks: Initial response period; clinicians typically assess for ≥5% weight loss to determine treatment continuation
Months 4-6: Continued gradual reduction with consistent use
Months 6-12: Progressive weight loss approaching maximum effect
Beyond 12 months: Weight maintenance phase with ongoing treatment
Combining weight loss injections with resistance training and adequate protein intake (generally 1.2-1.6 grams per kilogram body weight daily, though this should be individualized, especially for patients with kidney disease) helps preserve muscle mass during weight reduction. Working with a registered dietitian is recommended for personalized nutrition guidance. Patients should understand that these medications facilitate fat loss indirectly through appetite control rather than directly accelerating fat metabolism, and results require patience and consistent adherence to treatment protocols. Most patients regain weight if medication is discontinued, highlighting the chronic nature of obesity management.
Weight loss injections carry specific safety considerations and potential adverse effects that patients and clinicians must understand before initiating treatment.
Common gastrointestinal side effects affect the majority of patients, especially during dose escalation. These include nausea (occurring in 40-50% of patients), vomiting, diarrhea, constipation, and abdominal discomfort. These symptoms typically diminish over 4-8 weeks as tolerance develops. Starting with lower doses and gradually titrating upward, as recommended in FDA labeling, helps minimize these effects. Patients should be advised to eat smaller, more frequent meals and avoid high-fat foods that may exacerbate symptoms.
Serious but rare adverse events require clinical vigilance:
Pancreatitis: Patients should discontinue medication and seek immediate evaluation if experiencing severe, persistent abdominal pain radiating to the back
Gallbladder disease: Rapid weight loss increases cholelithiasis risk; symptoms include right upper quadrant pain, especially after meals
Hypoglycemia: Risk increases when combined with insulin or sulfonylureas; dose adjustments of concurrent medications may be necessary
Thyroid C-cell tumors: Observed in rodent studies; contraindicated in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2
Suicidality: Wegovy labeling includes monitoring for suicidal thoughts or behaviors
Important precautions and interactions:
Pregnancy: These medications should be discontinued before planned conception (semaglutide at least 2 months before; follow specific product labeling)
Contraception: Tirzepatide may reduce the effectiveness of oral hormonal contraceptives; patients should use non-oral or backup contraception for 4 weeks after initiation and each dose escalation
Gastroparesis: These medications may worsen symptoms in patients with pre-existing gastroparesis
Diabetic retinopathy: Patients with pre-existing retinopathy should be monitored by an ophthalmologist, particularly with rapid glycemic improvement
Dehydration: Persistent vomiting or diarrhea may lead to dehydration and worsen kidney function; patients should seek medical attention for severe or persistent GI symptoms
Regular monitoring during treatment should include assessment for adverse effects, weight loss progress, and metabolic parameters. Patients with diabetes require blood glucose monitoring, and those with other comorbidities may need specialized follow-up. Consultation with specialists in obesity medicine, endocrinology, or gastroenterology may be appropriate for complex cases or management of side effects.
Patients typically begin seeing weight reduction within the first few weeks, with significant fat loss developing over 4-6 months and peak effects occurring around 12 months of continuous treatment. Clinicians assess for at least 5% weight loss within the first 12-16 weeks to determine whether to continue treatment.
Most patients regain weight after discontinuing weight loss injections, as obesity is a chronic condition requiring ongoing management. These medications are typically intended for long-term use to maintain weight loss, and discontinuation should only occur under medical supervision.
Both contain semaglutide, but Ozempic is FDA-approved only for type 2 diabetes management at lower doses, while Wegovy is specifically approved for chronic weight management at higher doses. Using Ozempic for weight loss in patients without diabetes is considered off-label use.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.