LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Do you have to wean off tirzepatide when stopping treatment? Unlike medications that require gradual tapering to prevent withdrawal, tirzepatide does not need a formal weaning schedule. This dual GIP and GLP-1 receptor agonist, approved by the FDA as Mounjaro for type 2 diabetes and Zepbound for weight management, can be discontinued without a structured taper. However, stopping tirzepatide leads to predictable metabolic changes including weight regain and loss of glycemic control that require careful medical planning. Understanding the discontinuation process, potential consequences, and transition strategies is essential for maintaining the health improvements achieved during treatment.
Quick Answer: Tirzepatide does not require a formal tapering schedule when discontinuing treatment, as there is no physiological withdrawal syndrome associated with stopping.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (Mounjaro) and chronic weight management (Zepbound). This medication represents a novel therapeutic approach that targets two incretin hormone pathways simultaneously, offering enhanced glycemic control and significant weight reduction compared to single-receptor agonists.
The mechanism of action involves stimulating insulin secretion in a glucose-dependent manner, which means insulin release occurs primarily when blood glucose levels are elevated, thereby reducing the risk of hypoglycemia. Tirzepatide also suppresses glucagon secretion, slows gastric emptying, and reduces appetite through central nervous system pathways. These combined effects result in improved postprandial and fasting glucose levels, along with substantial weight loss that varies by indication and dose—typically 5-13% in type 2 diabetes trials and up to 15-20% in obesity trials at the highest doses (15 mg).
Administered as a once-weekly subcutaneous injection, tirzepatide is available in escalating doses from 2.5 mg to 15 mg. The medication requires dose titration over several weeks to minimize gastrointestinal adverse effects, which are the most commonly reported side effects. Common adverse reactions include nausea, diarrhea, vomiting, constipation, and abdominal discomfort, typically diminishing as the body adapts to the medication. Tirzepatide carries a boxed warning for thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2.
Understanding how tirzepatide works is essential when considering discontinuation, as its effects on glucose metabolism, gastric motility, and appetite regulation do not persist indefinitely after stopping treatment. The medication's half-life of approximately 5 days means that therapeutic effects gradually diminish over several weeks following the last dose.
Unlike certain medications such as corticosteroids, beta-blockers, or antidepressants that require gradual dose reduction to prevent withdrawal syndromes or rebound effects, tirzepatide does not require a formal tapering schedule when discontinuing treatment. The FDA-approved prescribing information for both Mounjaro and Zepbound does not mandate a specific weaning protocol, and there is no evidence of a physiological withdrawal syndrome associated with abrupt cessation.
However, the absence of a required taper does not mean discontinuation should occur without medical consultation. While you can technically stop tirzepatide immediately without physical harm from withdrawal, the metabolic and weight-related consequences of stopping require careful consideration and planning. Healthcare providers may recommend continuing treatment at a lower maintenance dose rather than complete cessation, particularly for patients who have achieved therapeutic goals.
Certain clinical scenarios might warrant a more gradual approach to discontinuation, even though not pharmacologically necessary. Patients experiencing significant gastrointestinal side effects might benefit from dose reduction before stopping entirely, and those with type 2 diabetes require transition planning to alternative glucose-lowering therapies. Patients taking insulin or sulfonylureas alongside tirzepatide need particular attention to avoid hyperglycemia when stopping. The decision to stop tirzepatide should always involve shared decision-making with your healthcare provider, considering individual circumstances, treatment goals, and the availability of alternative management strategies.
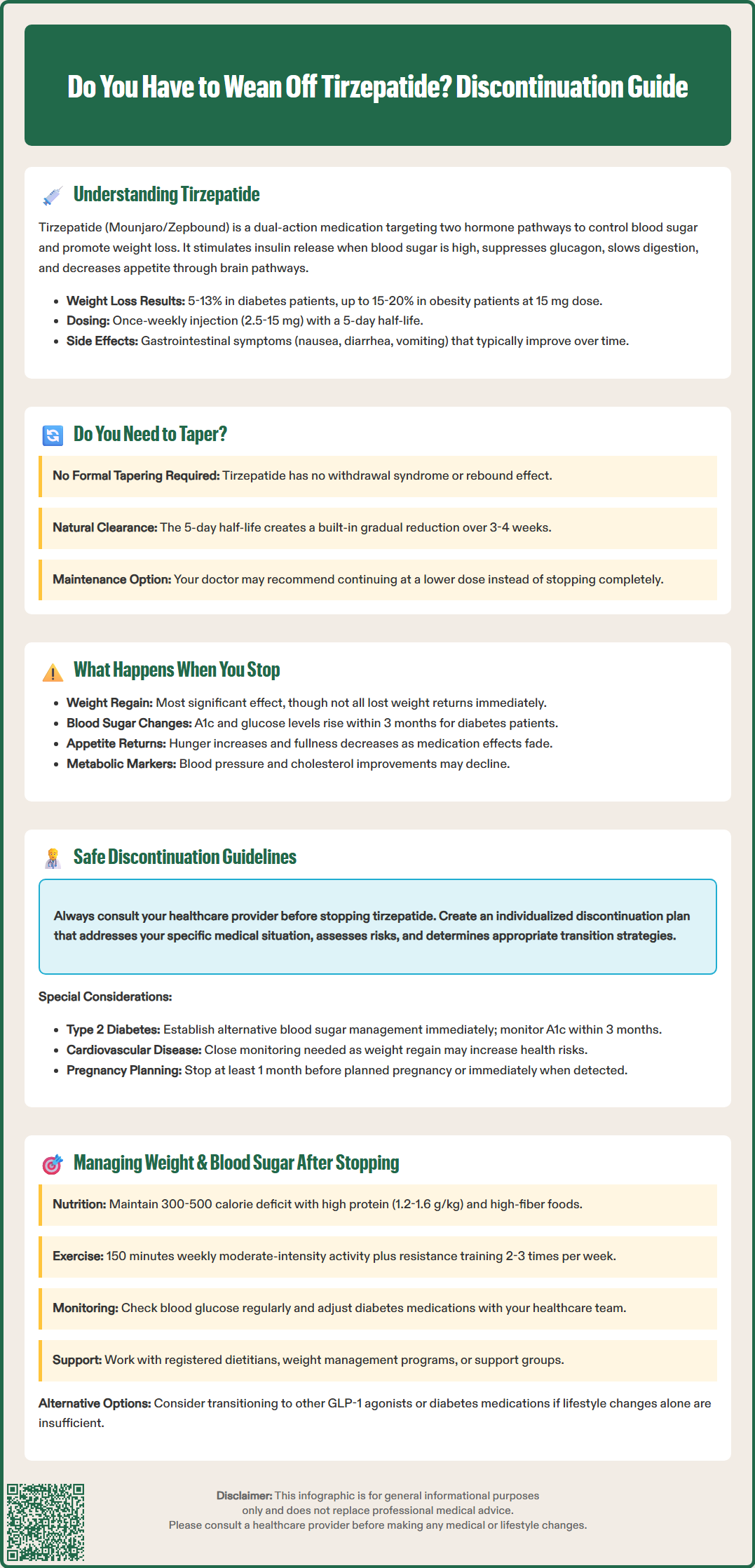
Discontinuing tirzepatide leads to predictable physiological changes as the medication's effects on incretin pathways, gastric motility, and appetite regulation gradually wane. The most significant and consistent finding is weight regain, which has been documented in clinical trials and real-world observations. The SURMOUNT-4 trial demonstrated that patients who discontinued tirzepatide after achieving weight loss regained significant weight compared to those who continued treatment, though not all weight loss was reversed during the study period.
For patients with type 2 diabetes, stopping tirzepatide results in loss of glycemic control unless alternative diabetes management strategies are implemented. Hemoglobin A1c levels typically rise within 3 months after discontinuation, and fasting and postprandial glucose levels increase as the medication's insulinotropic and glucagon-suppressing effects dissipate. The rate and magnitude of glycemic deterioration depend on individual factors including baseline diabetes severity, duration of disease, beta-cell function, and lifestyle factors.
Appetite changes represent another prominent effect of discontinuation. As tirzepatide's central appetite-suppressing effects fade, patients commonly experience increased hunger, return of food cravings, and changes in satiety signals. The medication's effect on gastric emptying also reverses, which may contribute to increased food intake and reduced feelings of fullness after meals. These changes can be psychologically challenging for patients who have become accustomed to reduced appetite during treatment.
Other metabolic parameters may also change after stopping tirzepatide, though individual responses vary. Some patients may experience changes in blood pressure, lipid profiles, and other cardiometabolic markers that had improved during treatment. These changes underscore that tirzepatide provides multifaceted cardiometabolic benefits beyond glucose and weight control, which may diminish upon discontinuation.
Importantly, there is no evidence of dangerous rebound effects or acute medical complications from stopping tirzepatide itself, but the loss of therapeutic benefits requires proactive management. Patients should seek urgent medical attention if they experience severe hyperglycemia (blood glucose >300 mg/dL), ketones in urine or blood, or symptoms of diabetic ketoacidosis (nausea, vomiting, abdominal pain, rapid breathing) after discontinuation.
Safe discontinuation of tirzepatide requires medical oversight and individualized planning, even though formal tapering is not pharmacologically necessary. Consultation with your healthcare provider before stopping is essential to assess the reasons for discontinuation, evaluate potential consequences, and develop an appropriate transition plan. Common reasons for stopping include achievement of weight goals, intolerable side effects, cost or access issues, pregnancy planning, or patient preference.
For patients with type 2 diabetes, the most critical consideration is ensuring continuity of glycemic control. Your healthcare provider should implement alternative diabetes management strategies before or immediately upon stopping tirzepatide. This may involve:
Initiating or optimizing other glucose-lowering medications such as metformin, SGLT2 inhibitors, or other GLP-1 receptor agonists
Intensifying lifestyle modifications including dietary changes and physical activity
Increasing frequency of blood glucose monitoring to detect deterioration early
Scheduling follow-up appointments to assess A1c levels within 3 months, per American Diabetes Association recommendations
Patients using tirzepatide solely for weight management face different considerations. Healthcare providers should discuss realistic expectations about weight maintenance after stopping and develop comprehensive strategies to minimize weight regain. This includes establishing sustainable dietary patterns, regular physical activity routines, behavioral support, and potentially considering alternative weight management medications if appropriate.
Certain clinical situations require particular caution when discontinuing tirzepatide. Patients with cardiovascular disease should have close monitoring, as weight regain and metabolic deterioration may affect cardiovascular risk. Those with a history of pancreatitis should be counseled that tirzepatide has not been studied in patients with a history of pancreatitis, and alternative therapies may be more appropriate. Patients should seek immediate medical attention for severe abdominal pain that could indicate pancreatitis.
Regarding pregnancy, tirzepatide is not recommended during pregnancy and should be discontinued when pregnancy is recognized or when planning pregnancy. Based on tirzepatide's half-life of approximately 5 days, discontinuation at least 1 month before a planned pregnancy is a common clinical recommendation, though specific timing should be individualized with healthcare provider guidance.
Documentation of the discontinuation plan, including reasons for stopping, transition strategies, and monitoring schedule, should be clearly communicated between patient and provider to ensure coordinated care and optimal outcomes.
Successfully managing weight and glycemic control after discontinuing tirzepatide requires proactive, multifaceted strategies that address the underlying metabolic and behavioral factors contributing to obesity and diabetes. Lifestyle modification becomes paramount when pharmacological support is withdrawn, and patients benefit from structured approaches rather than attempting to maintain results through willpower alone.
Dietary strategies should focus on sustainable, evidence-based approaches rather than restrictive dieting. Key principles include:
Maintaining a modest caloric deficit (300-500 calories below maintenance) to prevent rapid weight regain
Emphasizing protein intake (1.2-1.6 g/kg body weight) to preserve lean muscle mass and promote satiety, with individualization for those with chronic kidney disease or other conditions requiring protein modification
Incorporating high-fiber foods to enhance fullness and support glycemic control
Practicing mindful eating and portion awareness to compensate for increased appetite
Limiting ultra-processed foods and added sugars that promote overconsumption
Physical activity plays a crucial role in weight maintenance and glucose regulation after stopping tirzepatide. The American Diabetes Association and U.S. Department of Health and Human Services recommend at least 150 minutes of moderate-intensity aerobic activity weekly, combined with resistance training 2-3 times per week. Exercise helps maintain metabolic rate, preserves insulin sensitivity, and partially compensates for the loss of tirzepatide's metabolic effects. Increasing non-exercise activity thermogenesis through daily movement also contributes to energy expenditure.
For diabetes management, regular self-monitoring of blood glucose becomes increasingly important after discontinuation. Patients should work with their healthcare team to establish appropriate monitoring frequency and target ranges based on ADA recommendations. Medication adjustments may be necessary as glucose patterns change, and some patients may require addition of new glucose-lowering agents or intensification of existing therapies. Continuous glucose monitoring systems can provide valuable insights into glycemic patterns and help guide management decisions.
Behavioral and psychological support significantly improves outcomes after stopping weight management medications. Consider:
Working with a registered dietitian for personalized nutrition counseling
Engaging in behavioral weight management programs or support groups
Addressing emotional eating patterns and developing alternative coping strategies
Setting realistic expectations and defining success beyond the number on the scale
Establishing regular self-weighing (weekly) to detect early weight regain and prompt intervention
Some patients may benefit from transitioning to alternative pharmacological therapies rather than complete cessation of medication support. Other GLP-1 receptor agonists, combination therapies, or different medication classes may provide continued benefits with different side effect profiles or cost structures. This decision should be made collaboratively with your healthcare provider based on individual circumstances, treatment goals, and available options. The key principle is that stopping tirzepatide does not mean abandoning comprehensive weight and diabetes management, but rather transitioning to alternative strategies that can sustain the health improvements achieved during treatment.
Yes, tirzepatide can be stopped suddenly without a formal tapering schedule, as there is no evidence of withdrawal syndrome. However, medical consultation is essential to manage the metabolic consequences including weight regain and loss of glycemic control.
Weight regain is the most consistent finding after discontinuing tirzepatide, as appetite suppression and metabolic effects fade. Clinical trials show significant weight regain occurs without continued treatment or alternative management strategies.
With a half-life of approximately 5 days, tirzepatide gradually clears from the system over 3-4 weeks after the final injection. This extended elimination provides a natural tapering effect as drug concentrations decline progressively.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.