LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide, marketed as Mounjaro for type 2 diabetes and Zepbound for weight management, is an FDA-approved dual GIP and GLP-1 receptor agonist that requires careful administration to maximize benefits and minimize risks. Understanding tirzepatide dos and don'ts is essential for safe, effective therapy. This comprehensive guide covers proper dosing schedules, injection techniques, critical contraindications, side effect management, and when to seek medical attention. Whether you're newly prescribed tirzepatide or seeking to optimize your current regimen, following evidence-based guidelines ensures you achieve the best possible outcomes while avoiding potentially serious complications.
Quick Answer: Tirzepatide requires following prescribed dose escalation, weekly injection schedules, and site rotation while avoiding use in patients with personal or family history of medullary thyroid carcinoma or MEN 2 syndrome.
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight management), tirzepatide represents a significant advancement in metabolic disease therapy due to its dual incretin receptor activity. It is not indicated for the treatment of type 1 diabetes.
The medication works through multiple complementary mechanisms. As a GIP receptor agonist, tirzepatide enhances insulin secretion in a glucose-dependent manner, meaning it stimulates insulin release only when blood glucose levels are elevated, thereby reducing the risk of hypoglycemia. Simultaneously, its GLP-1 receptor agonist activity suppresses glucagon secretion, slows gastric emptying, and promotes satiety through central appetite regulation. This dual action results in improved glycemic control and substantial weight reduction.
Clinical trials have demonstrated that tirzepatide produces dose-dependent reductions in hemoglobin A1c (HbA1c) of up to 2.5% in type 2 diabetes. Weight loss effects vary by population, with clinical trials showing up to 21-22% mean weight loss in obesity trials (non-diabetes patients) and lower percentages in type 2 diabetes patients, depending on dose. The medication is administered once weekly via subcutaneous injection and is available in escalating doses ranging from 2.5 mg to 15 mg.
The American Diabetes Association (ADA) Standards of Care emphasize individualized therapy selection, with GLP-1 receptor agonists considered preferred agents for many patients with type 2 diabetes who require additional glucose-lowering therapy beyond metformin, particularly those with established cardiovascular disease or chronic kidney disease. However, tirzepatide's cardiovascular outcomes data are still emerging, and no cardiovascular benefit claim appears on its FDA labeling at this time.
Understanding tirzepatide's pharmacology is essential for both clinicians and patients to optimize therapeutic outcomes while minimizing potential adverse effects. The medication's unique dual incretin activity distinguishes it from single-receptor GLP-1 agonists and contributes to its enhanced efficacy profile.
Do follow the prescribed dose escalation schedule. Tirzepatide therapy typically begins at 2.5 mg once weekly for four weeks, serving as an initial dose to improve gastrointestinal tolerability rather than as a therapeutic dose. Your healthcare provider will then increase the dose to 5 mg weekly, with potential further increases in 2.5 mg increments every four weeks based on glycemic response and tolerability. This gradual titration is critical for minimizing gastrointestinal side effects such as nausea, vomiting, and diarrhea.
Do inject tirzepatide on the same day each week. Consistency in administration timing helps maintain stable drug levels and establishes a routine that improves medication adherence. You may inject at any time of day, with or without meals, but maintaining the same weekly schedule is important. If necessary, you can change your injection day as long as the last dose was administered at least three days (72 hours) prior.
Do rotate injection sites systematically. Administer tirzepatide subcutaneously in the abdomen, thigh, or upper arm, rotating sites with each injection to prevent lipodystrophy (abnormal fat distribution) and injection site reactions. Avoid injecting into areas that are tender, bruised, red, or hard. All three approved injection sites are clinically acceptable for administration.
Do maintain regular follow-up appointments. Your healthcare provider should monitor your HbA1c, fasting glucose, renal function, and weight at appropriate intervals. The American Diabetes Association recommends checking HbA1c at least every three months until glycemic targets are achieved, then at least twice yearly thereafter. Additionally, inform your provider about any persistent gastrointestinal symptoms, as dose adjustment may be necessary.
Do stay well-hydrated, particularly during the initial weeks of therapy when gastrointestinal side effects are most common. Adequate fluid intake helps prevent dehydration secondary to nausea, vomiting, or diarrhea, which can precipitate acute kidney injury, especially in patients with pre-existing renal impairment.
Do inform your healthcare provider about any history of pancreatitis, gallbladder disease, or severe gastrointestinal disease (such as gastroparesis) before starting tirzepatide.
Do discuss contraception with your healthcare provider if you are of childbearing potential. Tirzepatide may reduce the effectiveness of oral contraceptives due to delayed gastric emptying. Consider using a non-oral method or additional contraception for 4 weeks after initiation and with each dose escalation.
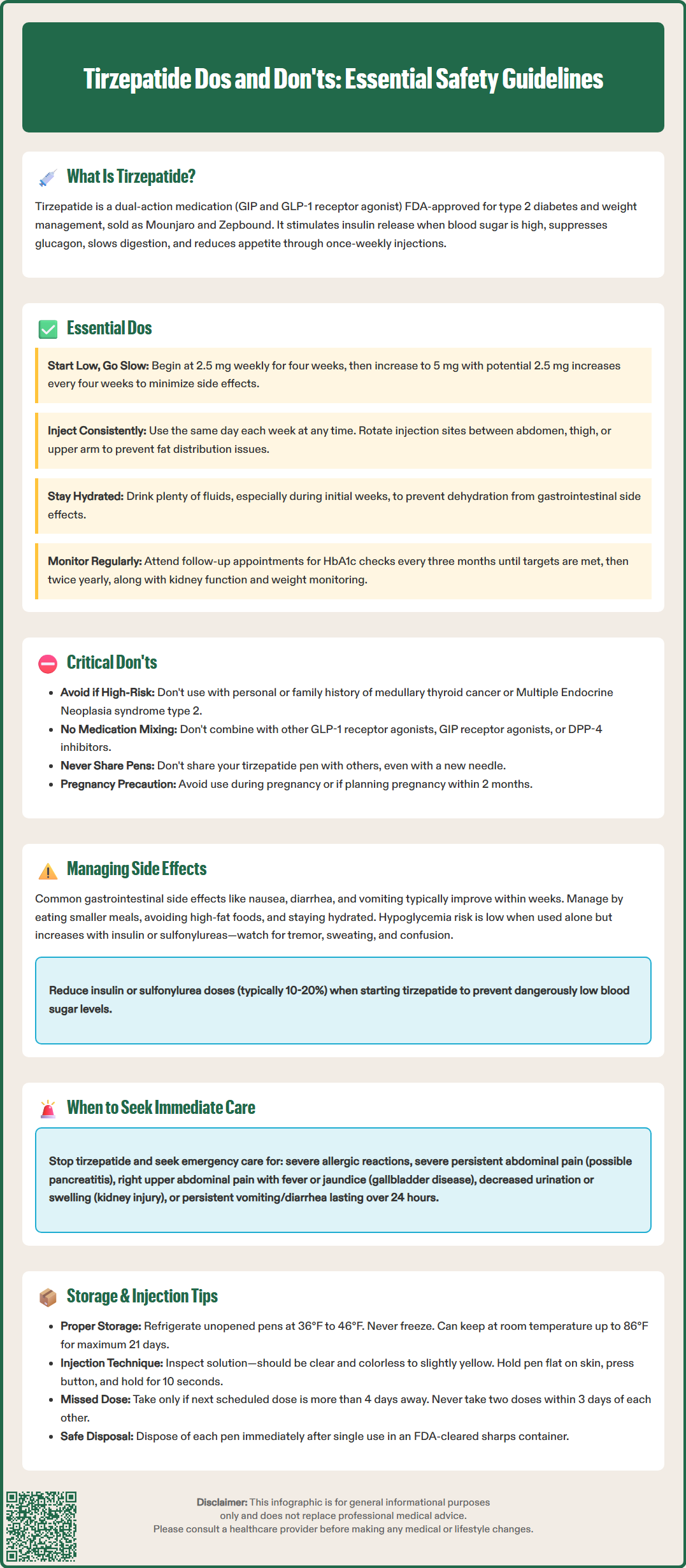
Don't use tirzepatide if you have a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). The FDA label carries a boxed warning regarding thyroid C-cell tumors observed in rodent studies. While causality in humans has not been established, tirzepatide is contraindicated in patients with these conditions. If you experience symptoms such as a neck mass, dysphagia, dyspnea, or persistent hoarseness, contact your healthcare provider immediately.
Don't use tirzepatide if you have a history of severe hypersensitivity reactions to tirzepatide or any excipients. Serious hypersensitivity reactions, including anaphylaxis and angioedema, have been reported. Discontinue tirzepatide immediately if such reactions occur and seek emergency medical attention.
Don't ignore symptoms of pancreatitis. Acute pancreatitis has been reported with GLP-1 receptor agonists, including tirzepatide. Discontinue tirzepatide promptly if you experience severe, persistent abdominal pain that may radiate to the back, with or without vomiting. Do not restart tirzepatide if pancreatitis is confirmed unless an alternative etiology is clearly identified.
Don't use tirzepatide with other GLP-1 receptor agonists or GIP receptor agonists. Concurrent use is not recommended as the safety and efficacy of such combinations have not been established. If transitioning from another incretin-based therapy, discontinue the previous agent before initiating tirzepatide.
Don't use tirzepatide with DPP-4 inhibitors. According to ADA Standards of Care, this combination provides no additional benefit and is not recommended.
Don't neglect to adjust concomitant diabetes medications. When adding tirzepatide to existing therapy, particularly insulin or sulfonylureas, dose reductions of these agents may be necessary to minimize hypoglycemia risk. The ADA recommends proactive insulin dose reduction (typically 10–20%) when initiating GLP-1 receptor agonist therapy in patients using basal insulin.
Don't use tirzepatide if you have severe gastrointestinal disease, such as severe gastroparesis, as it may worsen symptoms due to its effect on gastric emptying.
Don't use tirzepatide for weight management during pregnancy. Weight loss is not recommended during pregnancy, and Zepbound is not recommended for use in pregnancy. Discuss pregnancy plans with your healthcare provider, as weight loss medications should be discontinued at least 2 months before a planned pregnancy.
Don't share your tirzepatide pen with others, even if the needle is changed. Sharing injection devices poses a risk of transmission of blood-borne pathogens.
The most common adverse effects of tirzepatide are gastrointestinal in nature, with rates varying by dose and population. These include nausea, diarrhea, vomiting, constipation, abdominal pain, and dyspepsia. These symptoms are typically mild to moderate, transient, and most pronounced during dose escalation. To minimize gastrointestinal distress, eat smaller, more frequent meals, avoid high-fat foods, and ensure adequate hydration. Symptoms generally improve within several weeks as your body adjusts to the medication.
Hypoglycemia risk with tirzepatide monotherapy is low due to its glucose-dependent mechanism of action. However, when combined with insulin or sulfonylureas, the risk increases substantially. Recognize hypoglycemia symptoms including tremor, palpitations, sweating, confusion, and hunger. If you experience recurrent hypoglycemic episodes (blood glucose <70 mg/dL), contact your healthcare provider for medication adjustment.
Contact your doctor immediately if you experience:
Severe, persistent abdominal pain that may indicate pancreatitis, particularly if radiating to the back or accompanied by vomiting
Signs of gallbladder disease, including right upper quadrant pain, fever, jaundice, or clay-colored stools (cholelithiasis rates in clinical trials range from approximately 0.6% to 2.5%, depending on dose and duration)
Symptoms of acute kidney injury, such as decreased urination, swelling, fatigue, or confusion, especially if accompanied by dehydration
Visual changes, including blurred vision or difficulty focusing, which may indicate diabetic retinopathy complications (rapid glycemic improvement with tirzepatide can temporarily worsen retinopathy)
Severe allergic reactions, including rash, itching, swelling of face or throat, severe dizziness, or difficulty breathing
Persistent vomiting or diarrhea lasting more than 24 hours, which increases dehydration and acute kidney injury risk
Symptoms suggesting thyroid tumors, including neck mass, hoarseness, dysphagia, or dyspnea
New or worsening depression, suicidal thoughts, or unusual changes in mood or behavior, particularly in patients taking Zepbound for weight management
Routine monitoring should include periodic assessment of renal function, particularly in patients with pre-existing kidney disease or those experiencing significant gastrointestinal symptoms. Your healthcare provider may also recommend periodic lipase testing if pancreatitis is suspected, though routine monitoring is not indicated. Appropriate eye examinations should be scheduled, especially if you have pre-existing retinopathy.
Storage requirements: Store unopened tirzepatide pens in the refrigerator at 36°F to 46°F (2°C to 8°C). Do not freeze; if the medication has been frozen, discard it. Unopened pens may be kept at room temperature (up to 86°F or 30°C) for up to 21 days before use. Protect from light. Once a pen is used, it should be discarded immediately in an FDA-cleared sharps container.
Proper injection technique: Tirzepatide (Mounjaro and Zepbound) comes in single-dose, prefilled autoinjectors with hidden needles. Before injecting, inspect the solution through the pen window. Tirzepatide should be clear and colorless to slightly yellow; do not use if the solution is cloudy, discolored, or contains particles. Follow the manufacturer's Instructions for Use exactly. No needle attachment or priming is required. Clean the injection site with alcohol, remove the base cap, place the clear base flat against your skin at the injection site, unlock and press the gray injection button, and hold for 10 seconds. You will hear a click when the injection begins. After the injection is complete, the yellow indicator will fill the window, confirming the full dose was delivered. Remove from skin and dispose of the used pen immediately in an FDA-cleared sharps container.
Missed dose guidelines: If you miss a dose and the next scheduled dose is more than four days (96 hours) away, administer the missed dose as soon as possible. If the next scheduled dose is within four days (96 hours), skip the missed dose and resume your regular weekly schedule. Never administer two doses within three days (72 hours) of each other, as this increases the risk of gastrointestinal adverse effects and potential hypoglycemia.
Travel considerations: When traveling, unopened tirzepatide pens may be kept at room temperature (up to 86°F or 30°C) for up to 21 days. If traveling by air, keep tirzepatide in your carry-on luggage rather than checked baggage to avoid freezing temperatures in the cargo hold. Carry a letter from your healthcare provider documenting your prescription, particularly for international travel.
Disposal: Always dispose of used pens immediately after a single use in an FDA-cleared sharps disposal container, never in household trash or recycling bins. Follow local regulations for proper disposal of sharps containers.
Tirzepatide should not be combined with other GLP-1 receptor agonists, GIP agonists, or DPP-4 inhibitors. When used with insulin or sulfonylureas, dose reductions of these medications are typically necessary to prevent hypoglycemia, with insulin doses often reduced by 10–20% at initiation.
If your next scheduled dose is more than four days (96 hours) away, take the missed dose as soon as possible. If the next dose is within four days, skip the missed dose and resume your regular schedule. Never take two doses within three days (72 hours) of each other.
Tirzepatide is contraindicated in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2, those with severe hypersensitivity to tirzepatide, and should be used cautiously in patients with history of pancreatitis or severe gastrointestinal disease. It is not indicated for type 1 diabetes.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.