LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide injection site red and itchy reactions are commonly reported side effects of this dual GIP/GLP-1 receptor agonist medication. Approved by the FDA for type 2 diabetes and chronic weight management, tirzepatide (Mounjaro, Zepbound) is administered as a weekly subcutaneous injection. Localized redness, itching, swelling, or mild discomfort at injection sites typically occur as mild to moderate reactions that resolve within days. Understanding why these reactions happen, how to manage symptoms effectively, and when medical evaluation is necessary helps patients safely continue treatment while minimizing discomfort and maintaining optimal medication adherence.
Quick Answer: Tirzepatide injection site redness and itching are common, typically mild to moderate reactions caused by localized inflammation that usually resolve within 2-3 days without treatment discontinuation.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management and chronic weight management. Administered as a once-weekly subcutaneous injection, tirzepatide has demonstrated significant efficacy in glycemic control and weight reduction in clinical trials.
Injection site reactions are among the commonly reported adverse effects associated with tirzepatide therapy. According to the FDA prescribing information, these reactions vary by dose and product, typically manifesting as localized redness (erythema), itching (pruritus), swelling, or mild discomfort at the injection site. Most reactions are mild to moderate in severity and tend to resolve spontaneously within a few days without requiring treatment discontinuation.
Understanding that injection site reactions are a recognized adverse effect of tirzepatide can provide reassurance to patients experiencing these symptoms. The subcutaneous administration route inherently carries some risk of local tissue irritation, which may contribute to localized inflammatory responses in susceptible individuals.
While injection site reactions are generally self-limiting and not indicative of serious complications, patients should be educated about normal versus concerning symptoms. It's important to note that tirzepatide is contraindicated in patients with a personal or family history of serious hypersensitivity to tirzepatide or any of the product components. Recognizing the difference between expected mild reactions and signs requiring medical evaluation is essential for safe medication administration and optimal treatment adherence.
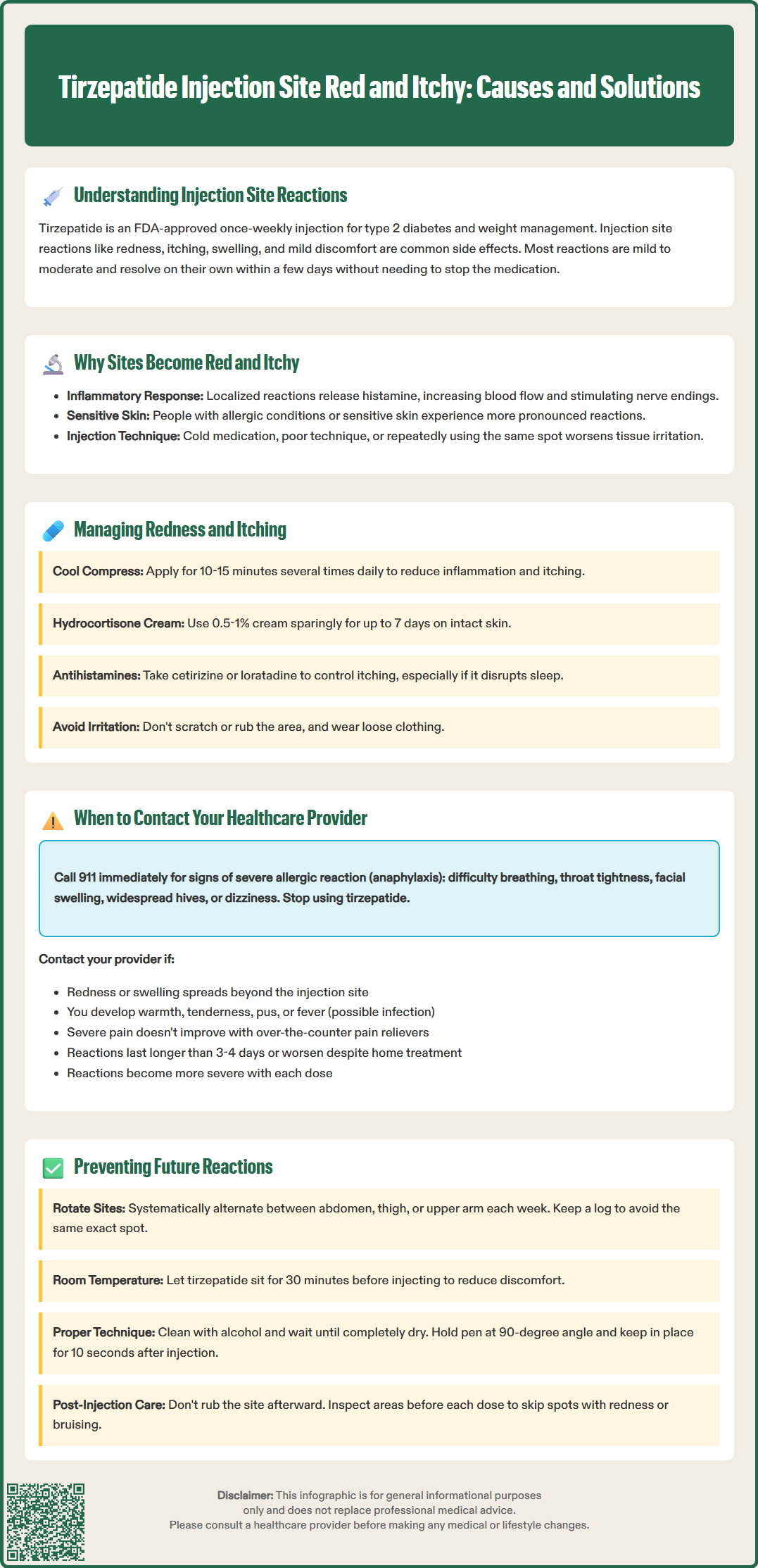
The development of redness and itching at tirzepatide injection sites results from several physiological mechanisms. When the medication is injected subcutaneously into the fatty tissue beneath the skin, it triggers a localized inflammatory response as part of the body's normal immune surveillance. This inflammatory cascade involves the release of histamine and other mediators from mast cells and basophils, which increase local blood flow (causing redness) and stimulate nerve endings (producing itching sensations).
Individual patient factors influence reaction susceptibility, including skin sensitivity, immune system reactivity, and previous exposure to similar medications. Patients with a history of allergic conditions or sensitive skin may experience more frequent or pronounced injection site reactions.
Mechanical factors during injection can exacerbate local irritation. Using cold medication directly from refrigeration (rather than allowing it to reach room temperature for approximately 30 minutes as recommended in the Instructions for Use), inadequate injection technique, or repeated injections in the same area can increase tissue trauma and inflammatory responses. While uncommon with GLP-1 receptor agonists compared to insulin, repeated injections in the exact same spot could potentially lead to localized tissue changes or increased sensitivity.
It is important to distinguish between normal injection site reactions and true allergic responses. Mild, localized redness and itching that resolve within 2-3 days typically represent non-allergic inflammatory reactions. In contrast, immediate widespread reactions, progressive swelling, difficulty breathing, or systemic symptoms may indicate a more serious hypersensitivity reaction requiring urgent medical evaluation. Hypersensitivity reactions to tirzepatide, including anaphylaxis, have been reported in the FDA prescribing information.
Most mild injection site reactions can be effectively managed with conservative home-based interventions. Immediately after noticing redness or itching, patients should avoid scratching or rubbing the affected area, as this can worsen inflammation and potentially introduce bacteria, increasing infection risk. Gentle cleansing with mild soap and water is appropriate if the skin appears intact, but aggressive scrubbing should be avoided.
Symptomatic relief strategies include:
Cold compresses: Applying a clean, cool (not ice-cold) compress to the injection site for 10-15 minutes can reduce inflammation, constrict blood vessels to decrease redness, and provide soothing relief from itching. This can be repeated several times daily as needed.
Topical treatments: Over-the-counter hydrocortisone cream (0.5-1%) may be applied sparingly to reduce inflammation and itching if the skin is not broken. Use should be limited to 7 days or less unless directed otherwise by a healthcare provider. Antihistamine creams should generally be avoided due to potential for contact sensitization. Calamine lotion or colloidal oatmeal preparations can provide additional soothing effects.
Oral antihistamines: Non-sedating oral antihistamines such as cetirizine or loratadine may help control itching, particularly if it interferes with sleep or daily activities. Be aware that some antihistamines may cause drowsiness; avoid driving or operating machinery until you know how these medications affect you. Consult with a pharmacist or healthcare provider about potential drug interactions.
Loose clothing: Wearing loose-fitting clothing over the injection site prevents friction and irritation that could exacerbate symptoms.
Patients should continue their regular tirzepatide dosing schedule unless specifically instructed otherwise by their healthcare provider, but should avoid injecting into previously irritated areas. Most injection site reactions do not require treatment modification or discontinuation. However, maintaining a symptom diary documenting the location, severity, and duration of reactions can help identify patterns and inform discussions with healthcare providers about potential technique modifications or management strategies. If reactions persist beyond 3-4 days or progressively worsen despite conservative management, medical evaluation is warranted. Serious adverse reactions should be reported to the FDA MedWatch program.
While most injection site reactions are benign and self-limiting, certain signs and symptoms warrant prompt medical evaluation. Patients should contact their healthcare provider if they experience progressive worsening of redness or swelling beyond the immediate injection site area, as this may indicate spreading cellulitis or other infectious complications. The development of warmth, tenderness, purulent drainage, or fever suggests possible bacterial infection requiring antibiotic therapy.
Seek immediate medical attention for:
Signs of severe allergic reaction: Difficulty breathing, throat tightness, facial or tongue swelling, widespread hives, dizziness, or rapid heartbeat may indicate anaphylaxis, a medical emergency. Call 911 immediately, stop using tirzepatide, and seek emergency department evaluation. Anaphylaxis requires immediate treatment with epinephrine.
Severe or persistent pain: While mild discomfort is common, severe pain at the injection site that does not improve with over-the-counter analgesics or that interferes significantly with daily activities should be evaluated.
Skin changes: Development of blisters, skin breakdown, necrosis (tissue death), or significant bruising may indicate injection technique problems or rare adverse reactions.
Systemic symptoms: Fever, chills, malaise, or other systemic symptoms accompanying injection site reactions require medical assessment to rule out infection or hypersensitivity reactions.
Patients experiencing recurrent or increasingly severe injection site reactions with each dose should schedule a non-urgent appointment with their healthcare provider or diabetes educator. These patterns may indicate the need for injection technique review, consideration of alternative injection sites, or evaluation for potential medication hypersensitivity. Healthcare providers can assess whether the reactions represent true allergic phenomena versus irritant reactions, which have different management implications and may affect decisions about treatment continuation. Patients who have experienced a serious hypersensitivity reaction should not be rechallenged with tirzepatide unless under the direct supervision of an allergist or immunologist.
Implementing proper injection technique and preventive strategies can significantly reduce the frequency and severity of injection site reactions. Systematic site rotation is the cornerstone of prevention. Tirzepatide should be injected into the abdomen, thigh, or upper arm (upper arm injections typically require assistance from a caregiver), with patients choosing a different site each week and avoiding using the exact same spot for subsequent injections. Maintaining a written or digital log of injection sites helps ensure adequate rotation.
Optimal injection technique includes:
Temperature equilibration: Remove tirzepatide from refrigeration approximately 30 minutes before injection to allow it to reach room temperature, which reduces injection discomfort and tissue irritation.
Skin preparation: Clean the injection site with an alcohol swab and allow it to dry completely before injection. Injecting through wet alcohol can cause stinging and increase irritation.
Proper device use: Follow the Instructions for Use exactly. For Mounjaro and Zepbound pens, place the pen flat against the skin at a 90-degree angle, press and hold until the indicator shows the dose is complete or you hear the second click, then hold for about 10 seconds before removing.
Inspection: Before each use, inspect the pen to ensure the solution is clear and free of particles. Do not use if the solution appears cloudy, discolored, or contains particles.
Post-injection care: Do not rub the injection site after administration, as this can increase local irritation and potentially affect medication absorption.
Patients should inspect potential injection sites before each dose, avoiding areas with existing redness, bruising, scarring, or skin abnormalities. Maintaining adequate hydration and healthy skin through regular moisturization (avoiding the immediate injection site area) may improve tissue resilience. For patients with recurrent reactions despite optimal technique, consultation with a diabetes educator or nurse specialist for hands-on injection training can be valuable. Never share tirzepatide pens with others, even if the needle has been changed, as this poses serious infection risks.
Most tirzepatide injection site reactions are mild to moderate and resolve spontaneously within 2-3 days without requiring treatment. If redness or itching persists beyond 3-4 days or progressively worsens, contact your healthcare provider for evaluation.
Yes, most patients can continue their regular tirzepatide dosing schedule with mild injection site reactions, but should inject into a different site away from the irritated area. Discontinue only if experiencing signs of severe allergic reaction or if specifically instructed by your healthcare provider.
Normal reactions involve mild, localized redness and itching that resolve within 2-3 days. Allergic reactions may include immediate widespread hives, progressive swelling beyond the injection site, difficulty breathing, throat tightness, facial swelling, or systemic symptoms requiring emergency medical attention.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.